Anticoagulants Explained: When and Why They Are Used
Blood clotting is a natural and crucial response of the body to prevent excessive bleeding when there is an injury or a cut. This process, known as the coagulation cascade, involves a complex series of steps that help the blood to form clots. However, blood clots that form inside blood vessels can be dangerous, as they may lead to serious conditions such as strokes, heart attacks, or pulmonary embolisms by obstructing normal blood flow.
Anticoagulants, commonly referred to as blood thinners, are used to prevent these dangerous types of clots. These medications are prescribed for individuals at high risk of forming abnormal blood clots due to conditions like atrial fibrillation (an irregular heartbeat), deep vein thrombosis (DVT), or those who have already suffered a heart attack or stroke. Anticoagulants work by interfering with the coagulation cascade to reduce the blood's ability to clot. This helps to lower the risk of clot-related complications in susceptible individuals.
Understanding Coagulation
Coagulation is defined as the formation of blood clots to seal wounds and stop bleeding. Several triggers can initiate coagulation, such as damage to the lining of blood vessels, a slowdown or cessation of blood flow (stasis), or the presence of conditions that favor clot formation (prothrombotic factors).
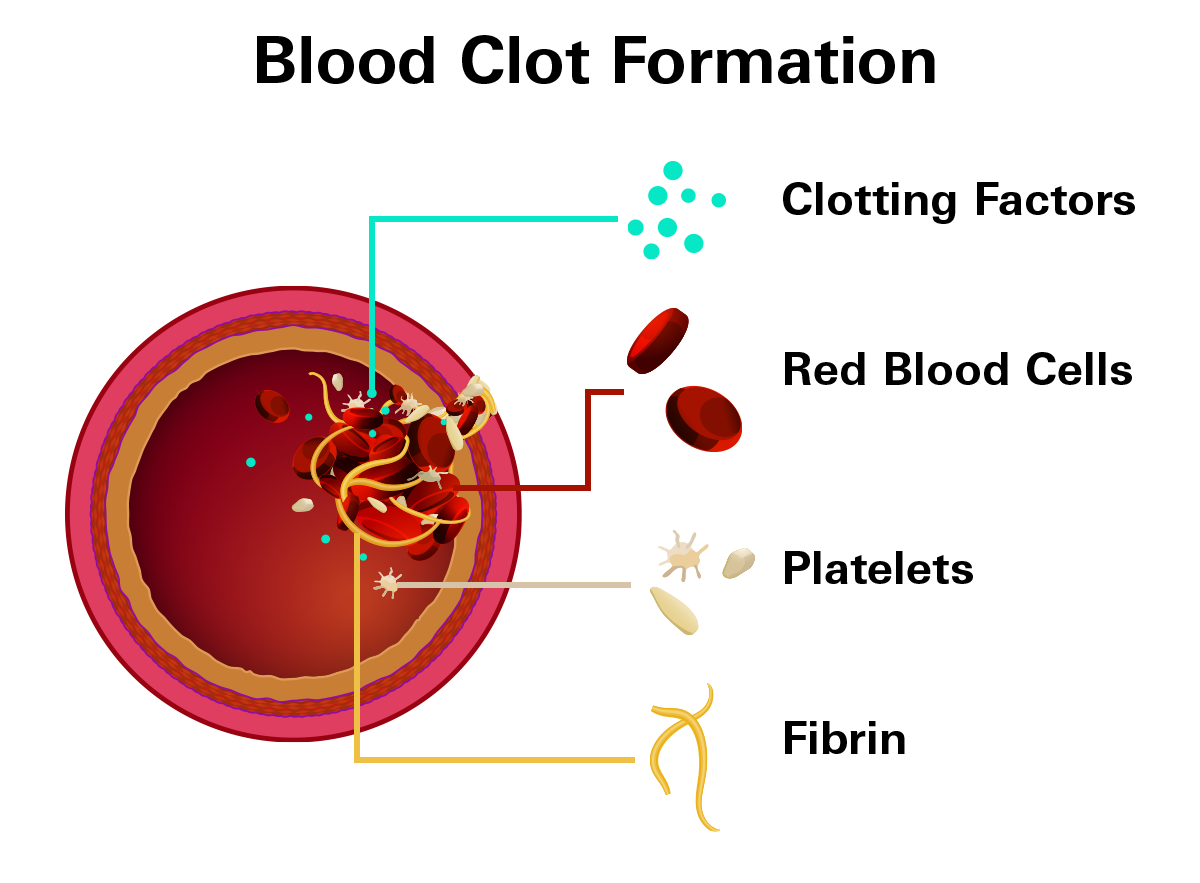
The process involves a complex series of events known as the coagulation cascade, where each clotting factor (a specialized protein in the blood) activates the next in a domino effect. This cascade occurs through two main pathways:
- Intrinsic Pathway (Contact Activation Pathway): This pathway is typically initiated by internal trauma within the vascular system.
- Extrinsic Pathway (Tissue Factor Pathway): This pathway begins when external trauma causes blood to escape the vascular system and interact with tissues outside the blood vessels.
Both pathways lead to the production of fibrin, a fibrous protein that weaves through the clot, providing structure and stability.
Role of Platelets
Platelets, small blood cells, are first responders to a site of injury. They adhere to the damaged area and to each other, forming a temporary plug. Platelets also release chemicals that activate the coagulation cascade, enhancing the production of a robust fibrin mesh.
Effect of Anticoagulants on the Coagulation Cascade
By targeting specific steps in the coagulation cascade, anticoagulants reduce the formation of fibrin and thus blood clots. This intervention is particularly important in conditions where the risk of clot formation is high, such as atrial fibrillation, deep vein thrombosis, or pulmonary embolism.
Key Uses of Anticoagulants
Anticoagulants are critical in managing certain conditions to reduce the risk of clots that can cause severe health issues.
- Acute Coronary Syndrome (ACS)
A medical condition involving an abrupt decrease or obstruction of your heart's blood flow, including heart attacks. - Atrial Fibrillation (AF)
A medical condition involving an irregular, frequently fast heartbeat that results in inadequate blood flow. - Myocardial Infarction (Heart Attack)
This occurs when blood flow to a part of the heart is blocked for a long enough time that part of the heart muscle is damaged or dies. - Unstable Angina (Chest Pain or Discomfort)
A medical condition in which your heart doesn't get enough blood flow and oxygen. It may lead to a heart attack. - Hip and Knee Replacement Surgery
Anticoagulants are used to prevent blood clots in the legs or lungs after these types of surgeries. - Prevention of Cardioembolic Stroke
This refers to a stroke caused by a blood clot that forms in the heart and travels to the brain, usually in people who do not have underlying cerebrovascular disease. - Venous Thromboembolism (VTE)
This includes conditions where blood clots form in the veins:
Deep Vein Thrombosis (DVT): Clots typically form in the deep veins of the legs, which can cause pain and swelling.
Pulmonary Embolism (PE): Clots that travel to the lungs and block one or more arteries, which can be life-threatening.
Examples of Anticoagulant Medications
There are several forms of anticoagulants. Each kind operates on the blood coagulation pathway at a different level.
Vitamin K Antagonists
Example: Warfarin (Brands: Coumadin, Jantoven)
How It Works: Vitamin K is essential for the activation of clotting factors II, VII, IX, and X, which are proteins that help blood clot. Warfarin works by reducing the activity of these vitamin K-dependent clotting factors, thereby slowing down the clotting process.
Monitering: Regular blood tests, such as the prothrombin time (PT) test to measure your International Normalized Ratio (INR), are necessary to ensure that warfarin is working effectively. The INR allows doctors to adjust the dose of warfarin to keep the patient’s clotting time within a safe and effective range. The target INR ranges between 2.0 and 3.0.
A high INR indicates a higher risk of bleeding, while a low INR suggests a higher risk of clotting. Maintaining an INR within the target range minimizes these risks.
Interactions: Warfarin requires monitoring of dietary vitamin K intake (found in green leafy vegetables like spinach and kale) as it can affect drug efficacy.
- Drugs that increase bleeding risk: NSAIDs, anti-platelet medications, SSRIs, and SNRIs
- Drugs that increase clotting risk: Estrogens, selective estrogen receptor modulators (SERMs).
- Medications that increase INR (Higher risk of bleeding): Carbamazepine, phenobarbital, phenytoin, rifampin, vitamin K in your diets, such as broccoli, brussel spouts, cabbage, lettuce, spinach, and green or black tea.
- Medications that decrease INR (Higher risk of clotting): Amiodarone, metronidazole, bactrim, anti-fungal medications, such as fluconazole, ketoconazole, and voriconazole.
Side Effects and Warnings: Common side effects include bleeding, skin necrosis, and purple toe syndrome. Due to its potential to cause serious bleeding, Warfarin carries a "Black Box Warning," the strictest warning issued by the FDA for prescription drugs.
Direct Factor Xa Inhibitors (DOACs: Direct Oral Anticoagulants)
How It Works: Direct Factor Xa Inhibitors, also known as DOACs or NOACs (new oral anticoagulants have less need for monitoring compared to warfarin. These drugs work by inhibiting Factor Xa, a key enzyme in the coagulation process that converts prothrombin to thrombin, crucial for forming blood clots.
Key Advantages of DOACs
- Efficiency: DOACs are effective at preventing strokes, particularly in conditions like atrial fibrillation that is not related to heart valve issues.
- Convenience: They require less frequent blood testing and have fewer dietary restrictions than warfarin.
- Speed: These medications act quickly and are also eliminated from the body faster than warfarin, which can be beneficial in managing dosing and side effects.
Medications and Dosage Information
- Apixaban (Eliquis):
For preventing stroke in atrial fibrillation: 5 mg twice daily.
For treating and preventing deep vein thrombosis (DVT) and pulmonary embolism (PE): Start with 10 mg twice daily for 7 days, then 5 mg twice daily.
After knee or hip replacement surgery to prevent DVT: 2.5 mg twice daily. - Rivaroxaban (Xarelto):
For stroke prevention in atrial fibrillation: 15-20 mg once daily with the evening meal.
For DVT and PE treatment: 15 mg twice daily for 21 days, then 20 mg once daily.
After knee or hip replacement surgery: 10 mg once daily, can be taken with or without food. - Edoxaban (Savaysa):
For stroke prevention in atrial fibrillation and treatment of DVT and PE: 30-60 mg once daily. - Betrixaban (Bevyxxa):
For preventing VTE in adults hospitalized for medical illnesses: Start with 160 mg once, followed by 80 mg daily with food for about 35-42 days.
Missed Doses: If a dose is missed, it should be taken as soon as possible on the same day. For doses of 15 mg twice daily (Rivaroxaban), both tablets can be taken at once if missed, then return to the regular schedule the next day.
Side Effects and Warnings:
- Bleeding risks, including gastrointestinal and urinary bleeding.
- Symptoms such as heavy menstrual bleeding, easy bruising, anemia, and changes in stool or urine color.
- Black Box Warning:
There is a risk of serious bleeding events which can be fatal. Individuals undergoing spinal procedures or receiving neuraxial anesthesia (such as an epidural) are at risk of developing spinal hematomas which could lead to paralysis.
Direct Thrombin Inhibitors: Dabigatran (Pradaxa)
How It Works: Direct thrombin inhibitors are a class of medication that specifically target thrombin (Factor IIa), a crucial enzyme in the blood clotting process. By binding directly to thrombin, these drugs prevent it from converting fibrinogen into fibrin, effectively reducing the formation of blood clots.
Primary Use: Dabigatran is primarily used to prevent stroke in patients with atrial fibrillation not caused by heart valve issues. It is also used for the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE).
Dosage
- For stroke prevention and treatment of DVT/PE: 150 mg taken twice daily.
- For preventing DVT/PE after hip replacement surgery: Start with 110 mg on the first day, followed by 220 mg once daily.
Administration
- How to Take: Dabigatran capsules should be swallowed whole with a full glass of water. The capsules should not be broken, chewed, or opened.
- Food: Dabigatran can be taken with or without food.
- Missed Dose: : If a dose is missed, take it as soon as possible on the same day. However, if it's within 6 hours of the next scheduled dose, skip the missed dose to avoid doubling up.
Side Effects and Warnings
- Common Side Effects: These include indigestion, stomach pain, nausea, diarrhea, and increased risk of gastrointestinal bleeding.
- Black Box Warning: Dabigatran has a significant warning for individuals receiving spinal injections or undergoing spinal procedures, as there is a risk of forming spinal hematomas that could lead to paralysis.
Important Precautions: Dabigatran is a potent anticoagulant that effectively reduces the risk of blood clot formation but also carries risks such as severe bleeding. It requires careful handling to ensure safety, particularly in patients with risk factors for bleeding or those undergoing certain medical procedures.
Speak With Your Doctor
Talk to your healthcare provider about which anticoagulant medication is best for you and send your prescription to Marley Drug. Save up to 95% compared to your local pharmacy by using Marley Drug.