Blood Thinners Don’t Really “Thin” Blood
Blood thinners, also known as anticoagulants, are medications that help prevent the formation of blood clots. They are commonly used to treat conditions involving the risk of blood clots, such as deep vein thrombosis (DVT), pulmonary embolism, atrial fibrillation, and certain heart conditions.
What are blood clots?
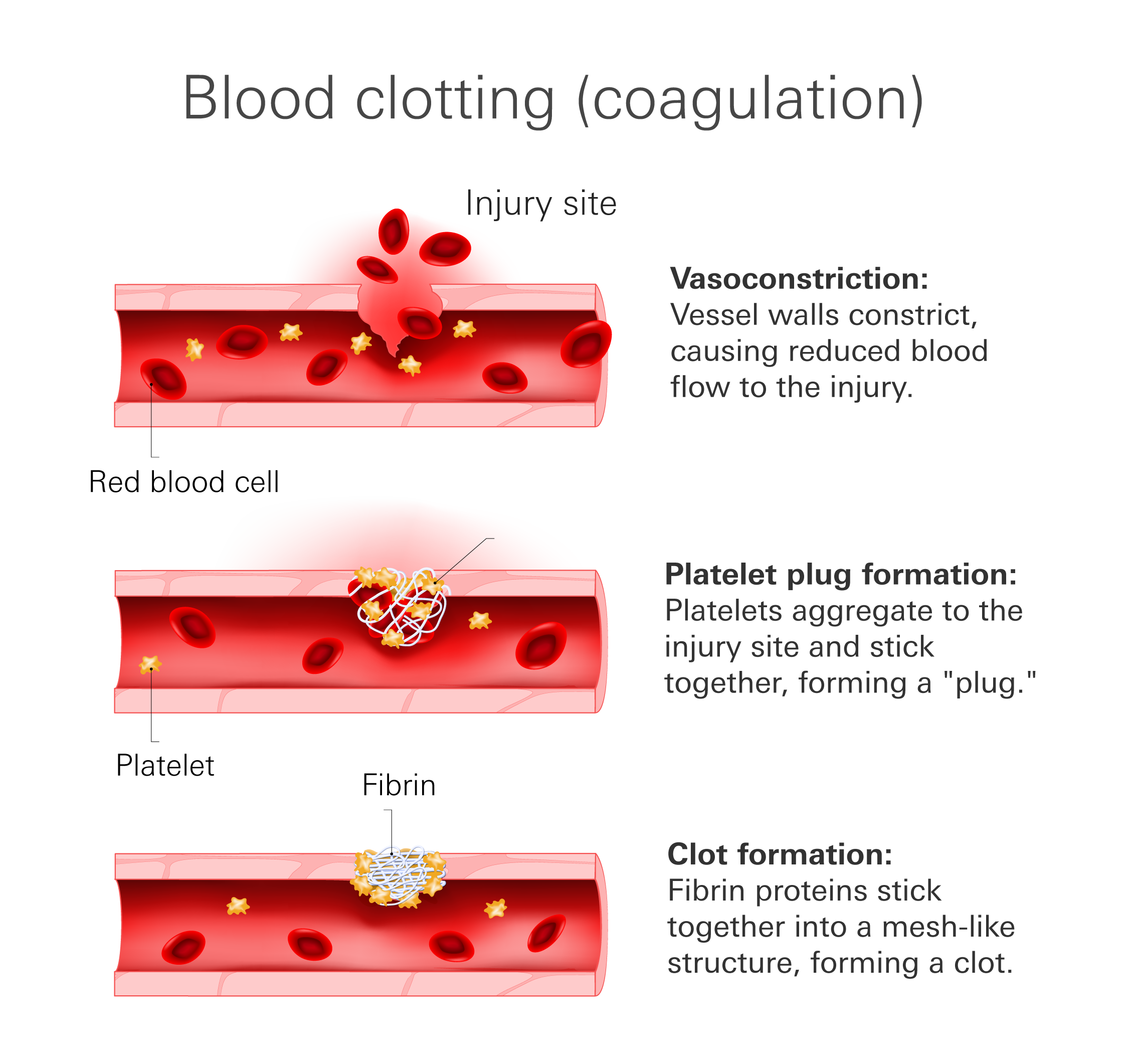
When you have a cut or injury, your body naturally forms a clot to stop the bleeding. This process involves a protein called thrombin that activates blood cells called platelets. These platelets gather at the site of the injury to create a plug that covers the wound. However, just the plug is not enough to completely stop bleeding. The clotting cascade takes place, forming a mesh-like structure called fibrin that reinforces the plug.
While blood clotting is essential for healing, sometimes it can occur in places where it shouldn't. This poses a danger because a clot inside a blood vessel can block the flow of blood, depriving the affected area of oxygen and nutrients. This can lead to tissue damage or death.
Unwanted blood clots are typically characterized by their location:
- Myocardial infarctions (MI) or “heart attack”, is a condition often caused by a blood clot blocking blood flow to the heart.
- Ischemic stroke is a condition caused by a blockage of blood flow to part of the brain.
- Pulmonary embolism (PE) is a blockage in the blood vessels of your lungs, often caused by a clot that has broken off elsewhere in the body and lodged itself in your lungs.
- Deep vein thrombosis (DVT) is a clot or “thrombosis” that occurs in one of the deep veins. This most often includes veins in your legs, pelvis, or sometimes arms.
How blood thinners work
Blood thinners work by interfering with the normal clotting process in your body. They do not actually "thin" your blood, but rather slow down the formation of clots. There are different types of blood thinners, but they all have a similar goal: to prevent clots from getting too big or forming in the wrong places.
Learn about Clotting Disorders
Blood thinners work by
- Decreasing the amount/activity of clotting factors in the blood
- Increasing the amount/activity of anti-clotting factors
It's important to note that blood thinners don't dissolve existing blood clots. They primarily focus on preventing the formation of new clots. In some cases, your body's natural clot-dissolving mechanisms can break down an existing clot over time, but this varies depending on the situation.
Blood thinners can also increase the risk of bleeding. Since blood clotting plays a crucial role in wound healing, even minor injuries can result in prolonged bleeding when you're on blood thinners.
- Minor bldding Minor bleeding is not dangerous. This could be extra bleeding while flossing, nose bleeds, and/or extra bleeding from cuts while shaving. This is relatively common. Minor bldding
- Major bleeding Major bleeding is a dangerous bleed that cannot be controlled at home with typical measures, and often involves major organs. Signs of a major bleed could include black tarry stools, vomiting blood, and/or blood in your urine. This is very uncommon, and if you are suspicious of any major bleeding it is imperative to seek medical care immediately.
Types of blood thinners
Bblood thinners by mechanism of action
| Medication | How it works | Effects |
| Warfarin | Inhibits the activity of vitamin K, which is necessary for certain clotting factors (Factors II, VII, IX, and X) in the liver. | Prolongs the time it takes for blood to clot. |
| Dabigatran
(Direct Oral Anticoagulant) |
Binds directly to thrombin, a key enzyme in the blood clotting cascade, and inhibit its activity. | Prevents the conversion of fibrinogen to fibrin and inhibit clot formation. |
| Rivaroxaban, apixaban, edoxaban
(Direct Oral Anticoagulants) |
Inhibit the activity of factor Xa, a crucial enzyme in the blood clotting pathway. | Prevent the conversion of prothrombin to thrombin, leading to reduced clot formation. |
| Heparin and Low Molecular Weight Heparin | Bind to antithrombin III, enhancing its activity to inactivate clotting factors. | Inhibit the formation of fibrin and prevent blood clotting. |
| Aspirin, clopidogrel, prasugrel, ticagrelor
(Antiplatelet agents) |
Inhibit platelet activation or aggregation, which are crucial steps in the formation of blood clots. | Reduce the risk of clot formation by inhibiting platelet function. |
Oral anticoagulants
Warfarin
Warfarin is the most common anticoagulant. It interferes with the action of vitamin K, which is essential for the synthesis of clotting factors in the liver. Without these factors, unwanted clots are much less likely to occur. With reduced levels of active clotting factors, the blood's ability to clot is impaired, making it less likely to form clots. This helps prevent the formation of harmful blood clots in conditions like atrial fibrillation, deep vein thrombosis (DVT), and pulmonary embolism.
Warfarin requires blood level monitoring to maintain the best possible dose and the ideal level of clotting control. Warfarin is often prescribed long-term for individuals who have experienced or are at high risk of experiencing a clot.
Side effects
- Minor bleeding
- Major bleeding
- Nausea
- Abdominal pain
- Purple/blackening of skin (if this occurs, it is essential you seek emergency medical case, as this is a sign of skin necrosis, or death of the skin tissue.)
It is important to note that there are many medications and foods, such as grapefruit, that interact with warfarin and should not be taken at the same time or otherwise need to be modified when used concurrently.
Direct Oral Anticoagulant (DOAC)s
DOACs, also known as novel oral anticoagulants, are a newer class of blood thinners. They include medications such as apixaban, dabigatran, edoxaban, and rivaroxaban.
DOACs directly target specific clotting factors in the blood, such as thrombin or factor Xa, which are key components of the clotting cascade and interfere with the clotting process to prevent the formation of blood clots.
How DOACs work
- Inhibition of Thrombin (Dabigatran)
Dabigatran is a DOAC that specifically targets thrombin, which is a crucial protein in the clotting process. Thrombin converts fibrinogen into fibrin, a protein that forms the mesh-like structure of a blood clot. By inhibiting thrombin, dabigatran prevents the formation of fibrin and therefore reduces the ability of the blood to clot. - Inhibition of Factor Xa (Apixaban, Edoxaban, Rivaroxaban)
Apixaban, edoxaban, and rivaroxaban target factor Xa, another important component of the clotting cascade. Factor Xa plays a critical role in the conversion of prothrombin to thrombin, which leads to the formation of fibrin and the subsequent clotting process. By inhibiting factor Xa, these DOACs prevent the formation of thrombin and fibrin, thereby reducing the blood's ability to clot.
The main advantage to DOACs is that they have quick onset and cessation of effect, so they can be quickly manipulated. They require less frequent blood monitoring by a healthcare provider, and fewer interactions with other medications. They are typically prescribed for prevention and/or treatment of clotting, such as DVTs and PEs.
Side effects
- Minor bleeding
- Major bleeding
- Nausea
- Vomitting
Aspirin
Though you may know aspirin as a medication used to treat headaches, the low dose of the medication is also commonly used as a blood thinner.
Aspirin is an anti-platelet medication. It works by inhibiting an enzyme called “COX-1” which is essential for platelet activation. Platelets are blood cells that get “sticky” when activated by signals of injury. These “sticky” platelets aggregate and help form the clot. Therefore, by preventing this platelet aggregation, aspirin helps to stop these clots from forming.
It is commonly prescribed to individuals at particularly high risk of experiencing clots or as an indefinite medication in individuals who have experienced heart-related events such as a heart attack.
Side effects
- Minor bleeding
- Major bleeding
- Stomach pain
- Heartburn
- Allergic reactions
Aspirin is not safe for everyone to take. Aspirin must be used cautiously or avoided altogether in certain circumstances:
- Concurrent use of other non-steroidal anti-inflammatory medications, such as ibuprofen (Advil)
- Those at increased risk of bleeding
- Concurrent use of other blood thinners
- Individuals under the age of 16
Anti-platelet Medications
Like aspirin, anti-platelet medications prevent platelets from getting “sticky” and coming together to form a clot. These medications, however, exert their effects at a different step in the platelet activation process, and are typically thought to be much stronger than aspirin.
Anti-platelet medications inhibit a receptor called “P2Y12”, and in doing so prevent platelets from becoming active. Examples of these medication include clopidogrel, ticagrelor, and prasugrel.
These medications are typically prescribed for 6–12 months following a heart-related event such as a heart attack. Additionally, if you have a stent put into a blood vessel they help to prevent a clot from forming around that stent.
Side effects
- Minor bleeding
- Major bleeding
- Headache
- Rash
- Heartburn
Injectable anticoagulant
Heparin
Heparin is usually administered by injection, either into a vein (intravenous heparin) or under the skin (subcutaneous heparin). It acts quickly and is often used in emergency situations or hospital settings, such as during surgeries, in the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), or for preventing clotting in certain medical conditions.
Heparin has a relatively short duration of action and requires continuous administration to maintain its anticoagulant effect. The dosage and duration of heparin therapy are determined by the patient's specific medical condition, blood clotting risks, and other factors. Close monitoring of the blood's clotting ability is necessary during heparin treatment to ensure the proper therapeutic range and minimize the risk of bleeding or clotting complications.
Heparin comes in two main forms:
Unfractionated heparin (UFH)
Unfractionated heparin is a mix of different sized heparin molecules that have antithrombin activity. Since it comes as a mix, UFH is more difficult to dose correctly and requires closer monitoring throughout treatment to ensure continued efficacy.
It is commonly used in acute settings, such as during surgeries, hemodialysis, and treatment of acute venous thromboembolism (VTE) or acute coronary syndromes (ACS).
A benefit of UFH is that, in the case of an overdose, its effects can be reversed with the administration of protamine sulphate. UFH is only given by IV, typically at a hospital.
Low molecular weight heparin (LMWH)
LMWH consists of smaller chains of heparin molecules. It has a longer half-life, allowing for once or twice-daily subcutaneous injections. LMWH has more predictable anticoagulant effects, which eliminates the need for routine monitoring of blood tests. This also decreased the risk of side effects.
This kind of heparin is dosed at home and is widely used for the prevention and treatment of VTE (venous thromboembolism).
Side effects specific to heparin
- Minor bleeding
- Major bleeding
- Injection site pain or irritation
- Heparin-induced thrombocytopenia (HIT)
HIT is an immune system reaction to heparin. It results in a decreased number of platelets in your blood. This condition greatly increases your risk of experiencing a blood clots and therefore can be very dangerous.
HIT is more common with UF than LMWH.
References
- Ahmed I, Majeed A, Powell R. Heparin induced thrombocytopenia: diagnosis and management update. Postgrad Med J. 2007 Sep;83(983):575-82. doi: 10.1136/pgmj.2007.059188. PMID: 17823223; PMCID: PMC2600013.
- Patel S, Singh R, Preuss CV, et al. Warfarin. [Updated 2023 Feb 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470313/
- Feng WH, Hsieh IC, Li YH. P2Y12 Inhibitor Monotherapy after Percutaneous Coronary Intervention: Is It Safe to Abandon Aspirin? Acta Cardiol Sin. 2021 Jan;37(1):1-8. doi: 10.6515/ACS.202101_37(1).20200806A. PMID: 33488022; PMCID: PMC7814326.
- Blood thinners: Benefits, risks, and how to use them. WebMD. Retrieved March 26, 2023, from https://www.webmd.com
- Daily aspirin therapy: Understand the benefits and risks. WebMD. Retrieved March 26, 2023, from https://www.webmd.com
- Mayo Foundation for Medical Education and Research. (2021, October 15). Should you take a daily aspirin for your heart? Mayo Clinic. Retrieved March 26, 2023, from https://www.mayoclinic.org
- Unfractionated vs. low-molecular-weight heparin for DVT. WebMD. Retrieved April 5, 2023, from https://www.webmd.com