Gluten-Free Living: Insights into Celiac Disease
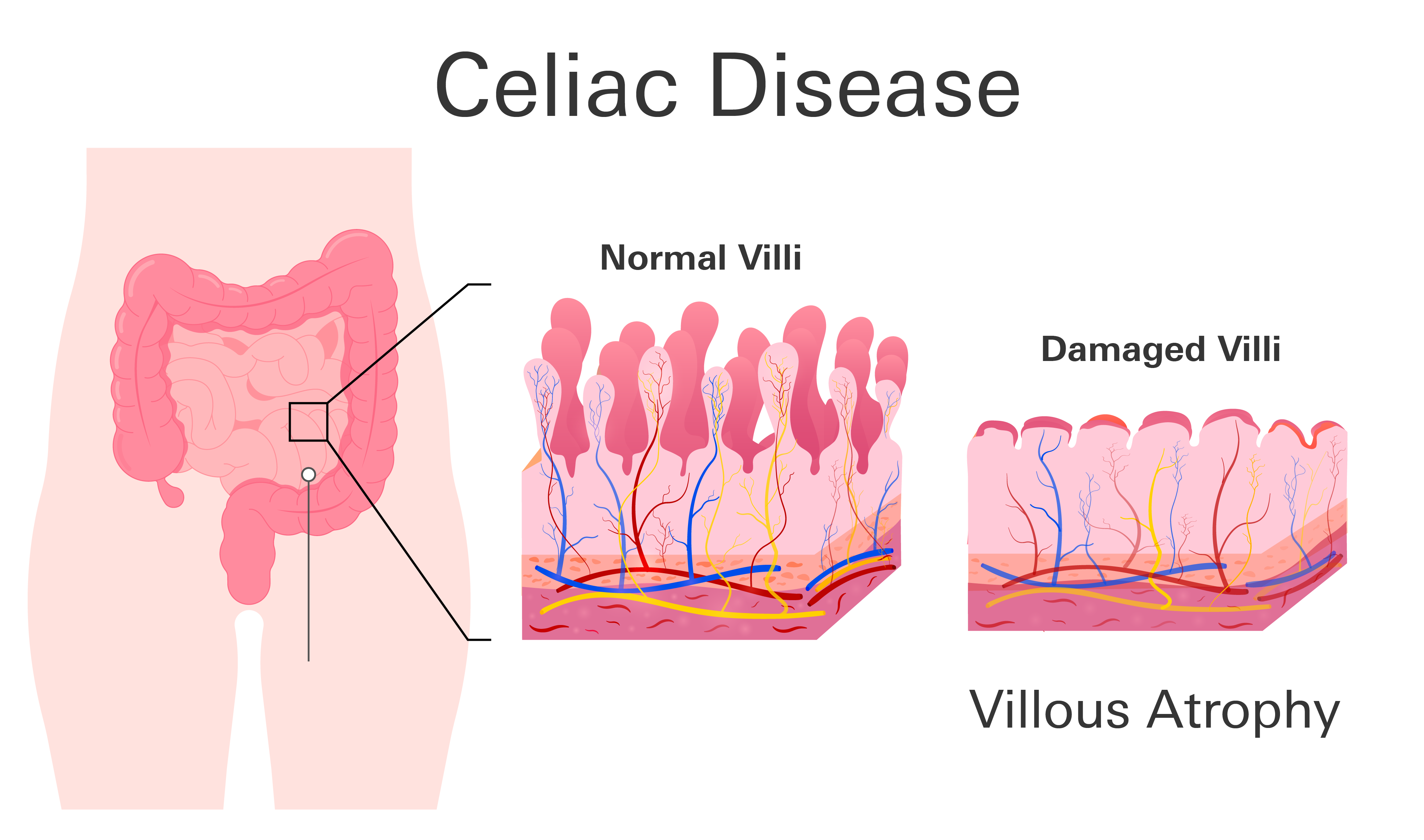
Celiac disease is a widespread autoimmune disorder, affecting about 1% of the U.S. population. It primarily targets the small intestine and is often set off by eating gluten, a protein found in wheat, barley, and rye. For those with this condition, gluten consumption triggers an abnormal immune response that attacks the small intestine's lining. This attack leads to a condition known as villous atrophy.
What is villous atrophy?
In the small intestine, there are tiny, finger-like projections called villi. These villi are critical for digesting food and absorbing nutrients, as they increase the intestine's surface area. In celiac disease, these villi become damaged and flattened, reducing their ability to absorb nutrients effectively. This damage, or atrophy, can lead to malabsorption, where the body struggles to absorb vital nutrients, causing various health issues like diarrhea, weight loss, anemia, and fatigue.
What causes celiac disease?
Celiac disease is caused by an interaction of genetic and environmental factors. People with certain genes (HLA-DQ2 and HLA-DQ8) are at risk. These genes are part of the body's immune system and are essential in how the body responds to gluten. Approximately 95% of people with celiac disease have the HLA-DQ2 gene, and most of the others have the HLA-DQ8 gene. Having these genes doesn't mean you will definitely develop celiac disease, but it does significantly increase your risk, especially if celiac disease runs in your family.
The combination of having these genetic markers and exposure to gluten is what leads to the development of celiac disease. However, it's important to note that not everyone with these genetic markers will develop the disease, suggesting that other environmental factors also play a role. Genetic testing can help determine if you have these markers and assess your risk, but it is not a definitive tool for diagnosing celiac disease on its own.
Signs and symptoms of celiac disease
There are several signs and symptoms of celiac disease that can occur and may differ from person to person.
- Digestive Issues: Diarrhea, nausea, vomiting, abdominal pain, bloating, constipation, unexplained weight loss
- Fatigue/Weakness: Persistent tiredness
- Skin Problems: Dermatitis Herpetiformis, skin blisters
- Joint Pain: Unexplained joint discomfort
- Neurological Symptoms: Headaches, peripheral neuropathy (numbness/tingling in extremities)
- Mood Disorders: Anxiety, depression, irritability
- Children's Symptoms: Delayed growth, puberty issues
- Reproductive Issues: Missed periods, infertility
- Mouth Ulcers: Canker sores
- Bone Health: Osteoporosis or osteopenia
Note that some people with celiac disease may have minimal or no digestive symptoms.
Dermatitis Herpetiformis
Gluten sensitivity, often linked with celiac disease, can also manifest in a less commonly known condition called Dermatitis Herpetiformis (DH). This skin condition is a direct result of the body's immune reaction to gluten, similar to how celiac disease affects the gut. DH primarily affects the skin, creating an uncomfortable and distinct symptom profile compared to celiac disease.
DH is characterized by a blistering, intensely itchy rash. This rash typically emerges on areas like the elbows, knees, torso, scalp, or buttocks. Unlike celiac disease, which is known for causing digestive issues, DH may not present any gastrointestinal symptoms. However, it is still a direct consequence of gluten sensitivity and shares an underlying immune response with celiac disease. The diagnosis and management of DH often require a careful consideration of diet and, in some cases, medication, similar to the approach for celiac disease.
Risk factors for celiac disease
Genetics
Genetics play a significant role: if you carry specific genetic markers, like the HLA-DQ2 or HLA-DQ8 genes, your chances of developing celiac disease are higher. For instance, having one copy of these genes gives you about a 3% risk, while having two copies can raise that risk to around 10%.
Family history
Your family background matters too. If a close family member, like a parent or sibling, has celiac disease, your risk increases. Also, people with other autoimmune disorders, such as type 1 diabetes or rheumatoid arthritis, are more likely to develop celiac disease.
Genetic conditions
Certain genetic conditions, like Down syndrome or Turner syndrome, are linked with a higher likelihood of having celiac disease. Additionally, some gastrointestinal issues, like irritable bowel syndrome (IBS) or microscopic colitis, may also increase your risk.
Early introduction to gluten
There’s also a discussion around how introducing gluten to infants affects celiac disease risk. Earlier, it was thought that introducing gluten either very early (before 3 months) or late (after 6 months) might increase the risk. However, more recent studies suggest that introducing gluten between 4 and 6 months might actually help prevent celiac disease, although this is still an area of ongoing research.
Remember, having these risk factors doesn't mean you'll definitely develop celiac disease. Likewise, it's possible to develop celiac disease without any of these factors. It's a complex condition influenced by a combination of genetic and environmental factors.
Is celiac disease temporary or preventable?
Celiac disease is a chronic and lifelong autoimmune disorder with no known cure. It requires a lifelong commitment to a gluten-free diet to manage symptoms and avoid complications. While this diet effectively manages the condition, it doesn't cure or prevent celiac disease. Early detection and proper dietary management are key to maintaining the health and wellbeing of individuals with celiac disease.
When to see a doctor
Consult a doctor for celiac disease if you have persistent digestive problems, unexplained fatigue, skin issues (like Dermatitis Herpetiformis), joint pain, iron-deficiency anemia, mood disorders, or a family history of the disease. It's crucial not to start a gluten-free diet before getting tested, as this can affect the accuracy of diagnostic tests. If these symptoms are present, seek medical advice for proper assessment and testing.
