Medications for COPD
What is COPD?
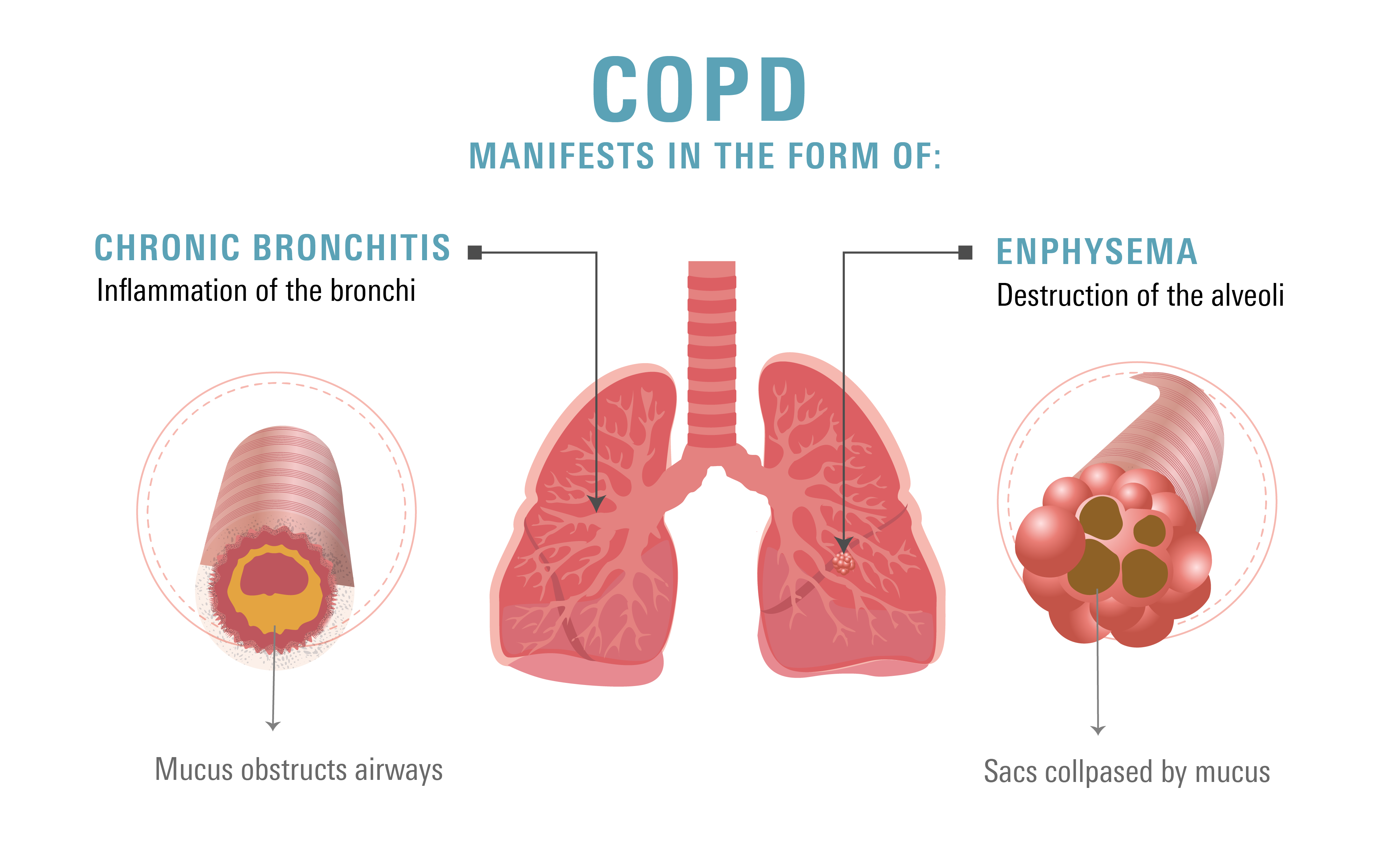
Chronic obstructive pulmonary disorder (COPD) is a long-term respiratory disease that causes obstructed airflow from your lungs.
The effects of COPD on your lungs cannot be revered and long-term progression or deterioration results in a steady loss of lung function.
It typically involves 2 conditions:
- Emphysema is defined as the destruction of the small passages/air sacs in your lungs called alveoli.
Your lungs may expand out and lose their springiness if your alveoli are damaged. You perience shortness of breath when the air becomes trapped in your lungs and you are unable to expel it.
- Chronic bronchitis is defined as inflammation and narrowing of your bronchi tubes, resulting in mucus production and a chronic cough.
May persist for at least 3 months for 2 years consecutively.
What Causes COPD?
The leading factor behind this condition is continuous exposure to allergens that inflame the lungs.
While tobacco smoke (a smoking history of at least 10 years) is the primary cause, COPD can also result from other air pollutant, including:
- Harmful particles
- Smoke from fires
- Cigars
- Pipes
- Marijuana
Long-term exposure to gases or particles leads to chronic inflammation in your lungs emphysema and/or bronchitis.
Signs and symptoms of COPD
You might not initially experience any symptoms. But if the condition worsens, you can get these COPD symptoms:
- Dyspnea (shortness of breath) that’s chronic and progressive/worsens overtime
- Chronic cough
- Excessive saliva and mucus production
- Blue fingerprints
- Wheezing
- Decreased energy
- Swollen ankles, feet, and/or legs
- Loss of weight
- Chest tightness
Individuals with COPD are also susceptible to exacerbations, in which symptoms worsen and last for at least a few days. If you have 2 or more exacerbations per year, you are considered to be a “frequent exacerbator.” Your risk of exacerbations increases as airflow limitations worsens.
Learn more about Asthma
How is COPD Treated?
Effective treatments can control your symptoms, delay disease progression, lower your risk of complications and exacerbations, and improve your ability to lead an active life, even for more advanced stages of COPD.
Smoking cessation is the only management strategy proven to slow the progression of COPD. You can prevent COPD from progressing and losing your ability to breathe by quitting smoking.
The symptoms and complications of COPD are treated with a variety of bronchodilator medications available as inhalers, including:
Short-acting beta-2 agonist (SABA)—used as needed
- Albuterol (ProAir HFA, ProAir RespiClick, Proventil HFA, Ventolin HFA, ProAir Digihaler): MDI/DPI: 1-2 inhalations every 4-6 hours as needed
- Levalbuterol (Xopenex, Xopenex concentration, Xopenex HFA): MDI: 1-2 inhalations every 4-6 hours as needed
- Epinephrine (Primatene mist): MDI: 1-2 inhalations every 4 hours as needed. Available as an over-the-counter (OTC) medication
Common side effects include:
- Nervousness
- Tremor
- Fast heart rate
- Palpitations
- Cough
- High blood sugar (hyperglycemia)
- High blood potassium levels
Short-acting muscarinic antagonist (SAMA)—used as needed
- Ipratropium Bromide (brand: Atrovent HFA): MDI: 2 inhalations four times a day
- Levalbuterol (Xopenex, Xopenex concentration, Xopenex HFA): MDI: 1-2 inhalations every 4-6 hours as needed
- Ipratropium Bromide + Albuterol (available as a brand: Combivent Respimat): MDI: 1 inhalation four times a day
Common side effects include:
- Dry mouth
- Upper respiratory tract infections
- Cough
- Bitter taste
Long-acting beta-2 agonists —if regular use is required
- Salmeterol (Serevent Diskus): DPI: 1 inhalation twice a day
- Salmeterol + Fluticasone (Advair Diskus, Wixela Inhub): DPI: 1 inhalation twice a day
- Formoterol (Perforomist): Nebulizer solution: 20 mcg twice a day
- Formoterol + Budesonide (Symbicort)
- Formoterol + Aclidinium (Duaklir Pressair)
- Formoterol + Glycopyrrolate (Bevespi Aerosphere)
- Arformoterol (Brovana): Nebulizer solution: 15 mcg twice a day
- Indacaterol (Arcapta Neohaler): DPI: 1 capsule via Neohaler device daily
This medication is a DPI that comes with a capsule that’s placed into the device. Do not swallow the capsule by mouth.
- Olodaterol (Striverdi Respimat): MDI: 1 inhalation daily
- Vilanterol + Umeclidinium (Anoro Ellipta)
- Vilanterol + Fluticasone (Breo Ellipta)
- Vilanterol + Umeclidinium/Fluticasone (Trelegy Ellipta)
Common side effects include:
- Nervousness
- Tremor
- Increased heart rate
- Palpitations
- Hyperglycemia (high blood sugar)
- Cough
- Low potassium
Long-acting muscarinic antagonists (LABA) —if regular use is required
- Long-acting muscarinic antagonists (LABA)
This medication is a DPI that has an indicator window that turns from green to red if the dose was inhaled properly.
- Aclidinium + Formoterol (Duaklir Pressair): DPI: 1 inhalation twice a day
- Glycopyrrolate (Seebri Neohaler): DPI: 1 capsule via Neohaler device twice a day
This medication is a DPI that comes with a capsule that’s placed into the device. Do not swallow the capsule by mouth.
- Revefenacin (Yupelri): Nebulizer: 175 mcg (1-unit dose vial) daily
- Umeclidinium (Incruse Ellipta): DPI: 1 inhalation daily
- Tiotropium (Spiriva Handihaler, Spiriva Respimat)
Spiriva Handihaler: DPI: 1 capsule via Handihaler device daily (requires 2 puffs). This medication is a DPI that comes with a capsule that’s placed into the device. Do not swallow the capsule by mouth.
Spiriva Respimat: MDI: 2 inhalations daily
Common side effects include:
- Dry mouth
- Upper respiratory tract infections
- Cough
- Bitter taste
Inhaled Corticosteroids (ICS)
Can be added to LABA treatment or LAMA/LABA treatment in particular individuals with past exacerbations and high blood eosinophils (eos) counts (a marker of inflammation).
can be added to LABA treatment or LAMA/LABA treatment in particular individuals with past exacerbations and high blood eosinophils (eos) counts (a marker of inflammation).
- Beclomethasone (QVAR RediHaler): MDI: 1-4 inhalations twice a day
- Budesonide (Pulmicort Flexhaler, Pulmicort Respules): DPI: 1-4 inhalations twice a day
- Ciclesonide (Alvesco): MDI: 1-2 inhalations twice a day
- Fluticasone (Flovent HFA, Flovent Diskus, Flovent Ellipta)
Flovent HFA: MDI: 2 inhalations twice a day
Flovent Diskus: DPI: 1-2 inhalations twice a day
Flovent Ellipta: DPI: 1-2 inhalations daily - Fluticasone + Salmeterol (Advair Diskus, Advair HFA, AirDuo RespiClick, Wixela Inhub)
- Mometasone (Asmanex HFA, Asmanex Twisthaler)
Asmanex HFA: MDI: 1-2 inhalations twice a day
Asmanex Twisthaler: DPI: 1-2 inhalations daily
Common side effects include:
- Difficulty speaking
- Cough
- Headache
- Hyperglycemia (high blood sugar)
- Hoarseness (raspy or strained voice)
- Oral candidiasis, also known as thrush
Oral thrush is a fungus infection in the mouth. To prevent oral thrush, rinse your mouth and throat with warm water and spit it out after each use, or use a spacer device if using an MDI.
- All metered dose inhalers (MDI) are aerosol-based inhalers and should be shaken well before use
- All dry powder inhalers (DPI) deliver medications to your lungs in the form of dry powder.
Speak with your doctor
There is no cure for COPD. The best way to prevent COPD from progressing is to take good care of yourself. Talk to your healthcare provider today and send your prescription to Marley Drug. Save up to 95% compared to your local pharmacy by using Marley Drug.