Parkinson's Disease - Causes, Symptoms, Diagnosis and Treatment Options
What is Parkinson’s disease?
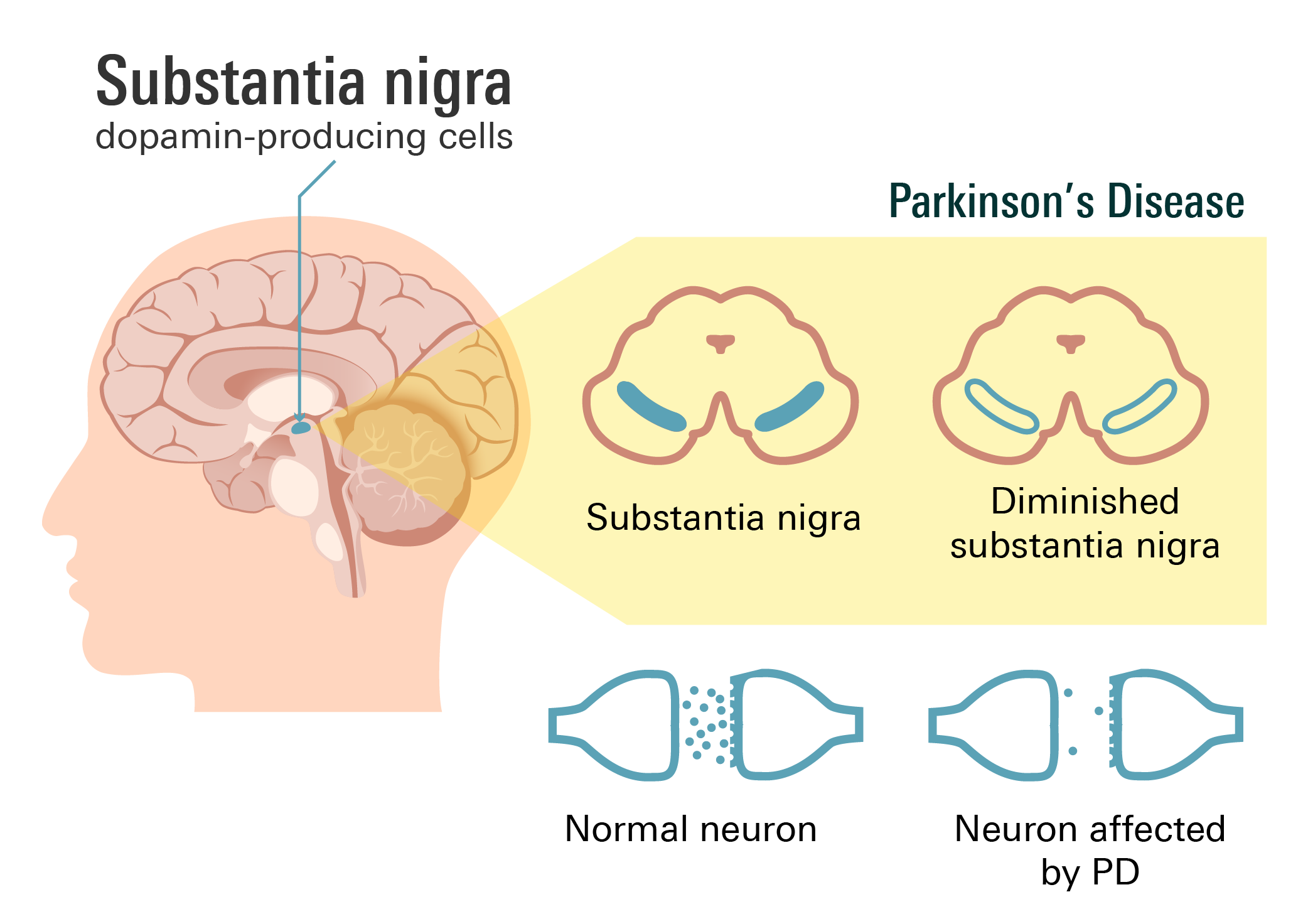
Parkinson’s disease, commonly abbreviated as “PD,” is a progressive neurological disorder that gradually develops over time and tends to affect your central nervous system. It’s often characterized by the degeneration of dopamine-producing cells in a specific region of your brain known as the substantia nigra.
Dopamine is a neurotransmitter that plays a crucial role in coordinating movement and controlling muscle activity. As the dopamine-producing cells gradually decline, the levels of dopamine in your brain decrease, leading to the characteristic motor symptoms of Parkinson's disease.
How common is Parkinson’s disease?
Parkinson's disease is the second most common neurological disorder after Alzheimer's disease.
This condition affects an estimated 1% to 2% of individuals over the age of 65 worldwide, according to the Parkinson's Foundation. In the United States, approximately 1 million Americans are currently living with Parkinson's disease, and around 60,000 new cases are diagnosed each year.
What causes Parkinson’s disease?
The exact cause of Parkinson's disease is not yet fully understood. However, researchers believe that a combination of genetic and environmental factors plays a role in its development. These include the following:
Genetic Factors
Certain genetic mutations and variations have been identified as risk factors for Parkinson's disease. These genetic factors are relatively rare and account for a small percentage of cases.
Dopamine deficiency
Parkinson's disease is characterized by the loss of dopamine-producing cells in your brain. Dopamine is a neurotransmitter that plays a crucial role in various bodily functions, including mood regulation, blood pressure control, and digestion. When someone has Parkinson's disease, there is a decrease in dopamine levels, which gives rise to a range of symptoms.
These symptoms can include tremors, difficulties with balance and walking, as well as slower and more rigid movements. The reduction in dopamine interferes with the normal functioning of neurons, resulting in the motor impairments characteristic of Parkinson's disease.
Environmental Factors
Exposure to certain environmental factors may contribute to the development of Parkinson's disease, especially in those with a genetic predisposition. These factors include exposure to toxins and chemicals, such as pesticides, herbicides, and industrial solvents.
Research suggests that prolonged exposure to these substances or certain occupations involving such exposures may increase the risk of developing Parkinson's disease.
Other Factors
Several other factors have been associated with an increased risk of this condition, although their exact contribution is not yet fully understood. These factors include age, as the risk increases with advancing age, gender, men are slightly more likely to develop Parkinson's than women, and certain head injuries.
While these factors are considered to play a role in the development of Parkinson's disease, it’s important to keep in mind that having these risk factors does not necessarily guarantee the onset of this condition. Many who possess genetic or environmental risk factors do not develop Parkinson's disease, while others who lack these factors can still be affected.
Parkinson’s disease symptoms
Parkinson's disease is characterized by a range of signs and symptoms that primarily affect your movement and motor function. These symptoms can vary in their presentation and severity from person to person.
The primary signs and symptoms of Parkinson's disease may include the following:
- Tremors: PInvoluntary shaking or trembling, often starting in your hands, fingers, thumbs, and/or chin. Tremors are generally more noticeable at rest and may decrease or disappear during purposeful movement.
- Akinesia or bradykinesia: Slowness of movement and difficulty initiating voluntary movements. Everyday tasks, including buttoning clothes, writing, and/or getting up from a chair, may become progressively challenging.
- Rigidity: Stiffness and resistance in your muscles, leading to a decreased range of motion. Keep in mind that this rigidity can cause muscle pain and impact your mobility.
- Postural instability: Impaired balance and coordination, leading to difficulties in maintaining an upright posture and an increased risk of falls.
- Changes in gait and walking: Parkinson's disease may cause changes in the way you walk, including a shuffling gait, reduced arm swing, and/or a tendency to take small steps. This can make walking and maintaining balance more challenging.
In addition to these primary motor symptoms, this condition can also present with various non- motor symptoms, which may appear before or alongside the motor symptoms or even in the later stages of the disease.
These non-motor symptoms may include the following:
- Cognitive changes: Problems with memory, attention, and/or executive function. Some individuals may develop dementia in the advanced stages of this disease.
- Mood alterations: Depression, anxiety, apathy, and/or irritability can occur.
- Sleep disturbances: Insomnia, excessive daytime sleepiness, and/or vivid dreams.
- Speech and swallowing difficulties:
- Sensory changes: Loss of sense of smell, also referred to as anosmia, or reduced sensitivity to various stimuli.
- Autonomic dysfunction: Symptoms such as constipation, urinary problems, and/or low blood pressure.
The progression and presentation of symptoms can differ from person to person in Parkinson's disease. As mentioned, not all individuals will experience every symptom, and the rate at which symptoms progress can vary as well.
If you or someone you know is exhibiting any of these signs or symptoms affiliated with Parkinson's disease, it’s recommended to seek medical advice and consult your healthcare professional for a thorough evaluation and accurate diagnosis. Your doctor will be able to assess your symptoms, perform appropriate tests, and provide appropriate guidance and treatment options.
How is Parkinson’s disease diagnosed?
The diagnosis of Parkinson's disease typically involves a comprehensive evaluation by a healthcare professional, often a neurologist with expertise in movement disorders.
Your diagnosis will generally be based on a combination of medical history, physical examination, and the presence of characteristic motor symptoms.
Medical history
During the diagnostic process for Parkinson's disease, your doctor will conduct an inquiry regarding your symptoms, including when they started, how they have progressed, and any factors that may be associated with their occurrence or exacerbation. They will also take a comprehensive medical history to identify any other existing medical conditions or medications that could potentially contribute to your symptoms.
This information is crucial in assessing the overall clinical picture and helps in distinguishing Parkinson's disease from other possible causes of similar symptoms.
Physical exam
A thorough physical exam will be conducted to assess motor symptoms associated with Parkinson's disease, including tremors, rigidity, bradykinesia, and postural instability.
Your doctor may also evaluate other aspects of the neurological exam, including reflexes, coordination, and/or sensory function, to rule out other possible causes of your symptoms.
Response to medications
In many cases, a positive response to medication can help support the diagnosis of Parkinson's disease. Your doctor may administer a trial of medication, typically Levodopa, to observe if there is an improvement in your motor symptoms.
Keep in mind that a positive response, although not definitive, can suggest Parkinson's disease as the underlying cause.
Additional tests
In some cases, additional tests may be conducted to help confirm the diagnosis or rule out other conditions that can mimic Parkinson's disease. These tests may include brain imaging techniques, including an MRI scan, to rule out other structural abnormalities.
Additionally, in 2011, the U.S. Food and Drug Administration (FDA) approved a diagnostic imaging scan known as dopamine transporter imaging, commonly abbreviated as the DaT scan, to enable doctors to obtain detailed images of your brain's dopamine system and assess dopamine levels in your brain.
Currently, there is no specific test or biomarker available that can provide a definitive diagnosis of Parkinson's disease. The diagnosis is primarily based on the presence of characteristic symptoms and the careful exclusion of other conditions that can manifest similar symptoms.
Therefore, it’s crucial to undergo a comprehensive evaluation conducted by a healthcare professional who specializes in movement disorders. This specialized assessment ensures a thorough review of symptoms and medical history and the ruling out of other potential causes. Therefore, by considering all relevant factors, an accurate diagnosis of Parkinson's disease can be established.
What are the risk factors of Parkinson’s disease?
The risk factors associated with Parkinson's disease can be divided into 2 main categories: genetic factors and environmental factors.
Some common risk factors associated with Parkinson's disease may include the following:
- Age: Advancing age is the most significant risk factor for Parkinson's disease. The risk of developing this condition increases significantly after the age of 60, although cases can occur in younger individuals as well.
- Genetics: Certain genetic mutations and variations have been linked to an increased risk of Parkinson's disease. However, as mentioned, it’s important to keep in mind that these genetic mutations are relatively rare and account for a small percentage of cases.
- Family history: Having a close relative, including a parent or sibling, with Parkinson's disease increases your chances of developing this condition. However, the overall risk remains relatively low unless there is a known genetic mutation associated with this disease..
- Environmental Factors: Exposure to certain environmental factors has been associated with an increased risk of developing this condition. These factors may include exposure to pesticides, herbicides, industrial chemicals, and toxins like solvents and heavy metals. However, the exact role and significance of these environmental factors in Parkinson's disease development require further research.
- Sex: Biological men have a slightly higher risk of developing Parkinson's disease compared to biological women. However, the reasons for this difference are not yet fully understood.
- Head trauma: Sustaining a significant head injury or multiple head injuries over time has been suggested as a possible risk factor for developing Parkinson's disease.
What are treatment options for Parkinson’s disease?
Treatment for Parkinson's disease often aims to alleviate your symptoms, improve your quality of life, and enhance daily functioning. The treatment plan is typically tailored to your specific needs and may involve medications, physical therapy, speech therapy, or supportive therapies.
Medications
Medications are commonly used to manage the symptoms of Parkinson's disease. Some medications often used for Parkinson’s disease may include the following:
Carbidopa/Levodopa (brand: Sinemet)
Levodopa is a prodrug that is converted to dopamine by DOPA decarboxylase and can cross your blood-brain barrier, making it the most effective drug because it compensates for dopamine deficiency.
Carbidopa is given with levodopa to prevent it from getting broken down during metabolism before it reaches your brain and provides efficacy.
Side effects:
- Nausea
- Dizziness
- Low blood pressure when standing up
- Dyskinesia
- Dry mouth
- Confusions
- Hallucinations
- Psychosis (disconnection from reality)
- Can cause brown, black, or dark discoloring of urine, saliva, and/or sweat, and can discolor clothing
Dopamine agonists
Pramipexole (Mirapex), Ropinirole (Requip), Rotigotine (Neupro) Patch
Side effects:
- Sleepiness
- Hallucinations
- Low blood pressure when standing up
- Dyskinesia
- Dizziness
- Nausea
- Vomiting
- Constipation
Monoamine oxidase-B inhibitor
Selegiline (Zelapar), Rasagiline (Azilect), Safinamide (Xadago)
Side effects:
- Hypertension
- Dyskinesia
- Headache
- Joint pain
- Indigestion
Physical therapy
This approach can be beneficial in managing mobility and improving your balance, flexibility, and strength.
Occupational therapy
This type of therapy focuses on improving daily living skills and adapting to your environment to enhance independence. Occupational therapists may suggest modifications to the home, recommend assistive devices, and provide strategies for managing activities of daily living.
Speech therapy
Speech therapy can help those with Parkinson's disease improve their communication skills. Your therapists may provide techniques to address difficulties in your speech volume, articulation, and/or swallowing.
Lifestyle modifications
Engaging in regular exercise, maintaining a healthy diet, and getting sufficient rest and sleep can have a positive impact on overall well-being and symptom management. A balanced diet rich in fruits, vegetables, and whole grains is also recommended.
Supportive therapies
Psychological counseling, support groups, and educational programs can provide emotional support, information, and strategies for coping with the challenges of living with this condition.
Seeking guidance from a healthcare professional, particularly a neurologist who specializes in movement disorders, is crucial for developing a personalized treatment plan for Parkinson's disease. As this condition is progressive and symptoms may evolve over time, regular consultations with your healthcare team allow for adjustments in your treatment approach.
Can Parkinson’s disease be prevented?
Unfortunately, there is currently no known way to prevent Parkinson's disease entirely. As mentioned, developing Parkinson's disease is thought to be influenced by a combination of genetic and environmental factors, many of which are beyond your control. However, certain lifestyle choices and habits have been suggested to potentially reduce your risk of developing this condition or even delaying its onset.
These suggestions include the following:
- Exercising regularly: Engaging in consistent physical activity has been affiliated with a decreased risk of Parkinson's disease. Activities such as walking, jogging, cycling, dancing, and/or any other form of exercise may be beneficial.
- Healthy diet: Consuming a well-balanced diet, rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, is generally recommended for overall health. Some research even suggests that a diet rich in antioxidants, such as vitamins C and E, may have a protective effect against Parkinson's disease.
- Avoiding environmental toxins as much as possible: Minimizing exposure to potential environmental toxins, including pesticides, herbicides, and industrial chemicals, may be beneficial. Take precautions in certain occupations or hobbies that involve exposure to these substances.
- Caffeine: Some studies have suggested a potential protective effect of caffeine against Parkinson's disease. Therefore, moderate consumption of caffeine, through sources like coffee or tea, may be associated with a lower risk.
- Smoking cessation: Smoking tobacco has been consistently linked to an increased risk of developing Parkinson's disease. Quitting smoking or avoiding tobacco products altogether is recommended for overall health benefits.
While these lifestyle recommendations may have potential benefits, it's important to note that they do not guarantee the prevention of Parkinson's disease. To make informed decisions regarding prevention, it’s recommended to consult with healthcare professionals who can provide personalized advice based on your specific circumstances.