What Depression Is
Depression is classified as a mood disorder that may be described as feelings of loss, anger or sadness that interfere with one’s everyday activities. An estimated 1 in 15 adults (6.7%) experience depression in a given year.
On average, depression first appears during the late teens to mid-20s, although it can occur at any time. It has been shown that one-third of women will experience a major depressive episode at least once in their lifetime. There is also a high degree of heritability (approximately 40%) when immediate relatives such as parents or siblings have depression.
See our blog on General Anxiety Disorder (GAD)
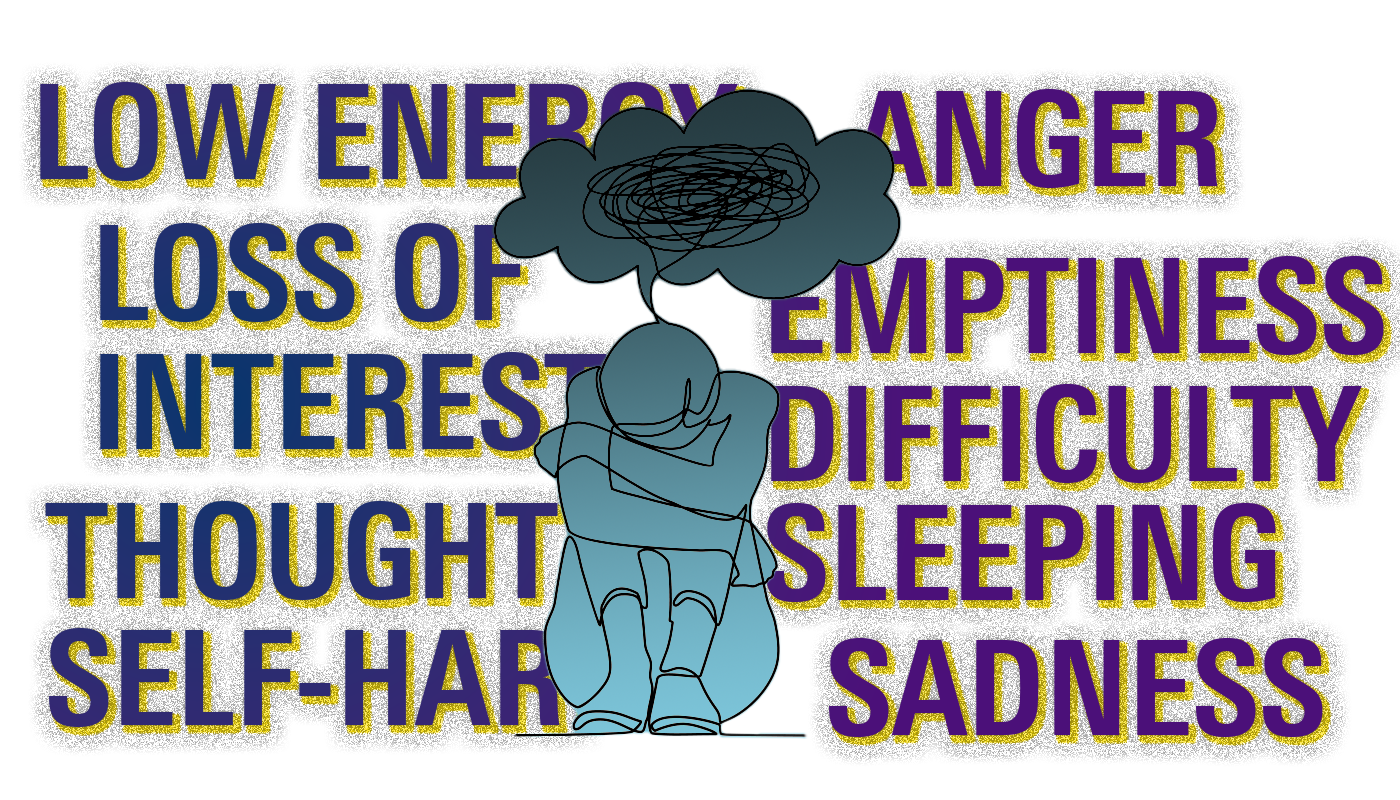
Signs and symptoms
Depression can appear in many different forms and usually depends on each individual person. They can vary in how often they appear, the severity of the symptoms, as well as how long these feelings last for. If you have experienced some of the following signs and symptoms nearly everyday for at least 2 weeks, you may be living with depression:
- Feeling sad or “empty”
- Feeling bothered, annoyed or angry
- A loss of interest in hobbies you once enjoyed
- Decreased energy levels
- Difficulty sleeping
- Thoughts of death, suicide or self-harm
Depression risk factors
There are many factors that can affect one’s risk of developing depression. These can be biochemical, medical, social, genetic or circumstantial in nature. Some common risk factors include:
- Sex: Females are at higher risk of developing depression than men.
- Genetics: You have a higher risk of developing depression if a family member has also had depression.
- Socioeconomic status: This includes financial problems and perceived low social status.
- Certain medications: These may include hormonal birth control, corticosteroids and beta-blockers.
- Vitamin D deficiency:Low levels of vitamin D have been linked to depressive symptoms.
- Gender identity: Transgender people have a risk of depression nearly 4-fold higher than cisgender people.
- Medical illness: People with heart disease are twice as likely to develop depression than people who don’t, and 1 in 4 people with cancer may experience depression.
Depression types
There are 2 major types of depression that differ by symptom severity and persistence.
Major depressive disorder (MDD): This is the more severe form of depression and is characterized by persistent feelings of sadness, hopelessness and worthlessness that will not go away on their own. In order to diagnose someone with clinical depression they must experience 5 or more of the following symptoms over a 2-week period:
- Feeling depressed most of the day
- Significant weight loss or gain
- Loss of interest in most regular activities
- Excessive sleeping or inability to sleep
- Slowed thinking or movement
- Fatigue most days
- Feelings of worthlessness or guilt
- Loss of concentration or indecisiveness
- Recurring thoughts of death or suicide
Persistent depressive disorder (PDD): This is a milder form of depression but it is more chronic. In order to be diagnosed with this disorder your symptoms must be present for at least 2 years. Since these symptoms last longer than MDD, it can have a larger impact on your life. It is very common for people with PDD to lose interest in normal daily activities, feel hopeless, have low self-esteem and lack productivity.
Postpartum depression: This is in a category of its own and usually refers to depression after childbirth. Postpartum depression affects 1 in 9 new parents. Surprising to most, this can affect both men and women. The symptoms usually appear 3-6 months after birth and if they last longer than 2 weeks you may be experiencing postpartum depression. Including the symptoms already listed previously you may also experience:
- Having thoughts of hurting the baby or yourself
- Not having an interest in the baby as if your baby is someone else’s
- Having memory problems
- Withdrawing from friends and family
Depression medication
Along with other treatments such as psychotherapy (talking to a therapist), medications are often prescribed to help alleviate some of the symptoms associated with depression. These include:
Selective serotonin reuptake inhibitors (SSRIs): These are the most commonly prescribed antidepressants because they tend to have fewer side effects. They treat depression by increasing the availability of the neurotransmitter's serotonin (happiness chemical). SSRIs include citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil) and sertraline (Zoloft).
Serotonin-norepinephrine reuptake inhibitors (SNRIs): These treat depression by increasing the amount of the neurotransmitter’s serotonin and norepinephrine in your brain. SNRIs include duloxetine (Cymbalta), desvenlafaxine (Khedezla) and venlafaxine (Effexor XR).
Tricyclic and tetracyclic antidepressants: Both of these treat depression by increasing the amount of the neurotransmitter’s serotonin and norepinephrine in the brain. These can be very effective but tend to cause more severe side effects, so they are generally not prescribed unless you’ve tried an SSRI first. Medications in this category include amitriptyline (Amitid), mirtazapine (Remeron) and nortriptyline (Pamelor).
Atypical antidepressant: These medications don’t fit into any of the other categories of antidepressants but they treat depression in a similar manner. These include bupropion (Wellbutrin) and trazodone (Desyrel).
When to see a doctor
Depression is a highly stigmatized disease that a lot of people do not seek treatment for, in fact, 1 in 6 people (16.6%) will experience it in their lifetime. Depression has a variety of symptoms that affect each individual differently.
If you feel depressed, or think you feel depressed, make an appointment with your healthcare provider as soon as you can. Talking about it is the first step to getting your mental health back on track.
Already taking one of these medications?
If you have already received help and are taking any of the medications listed above, check out our website!
Antidepressant list for $70/yearDesvenlafaxine $154.61/year
