Choosing the right statin for your lifestyle can be a daunting task. Use the guide below when discussing a statin therapy with your healthcare provider.
Atorvastatin is the Most Prescribed Medication in the U.S.
Statins are one the most widely prescribed medications worldwide, and atorvastatin is at the top of that list.
Statins, also known as HMG-CoA reductase inhibitors, are the recommended “first-line” medication to help reduce serum LDL levels (bad cholesterol).
Statins have decades worth of data and randomized clinical trials have found that treatment with statin therapy reduces the risk of heart disease.
According to the newest Blood Cholesterol Guidelines, statins are no longer just for lowering cholesterol, the focus is instead on each individual patient’s risk of having a heart attack and stroke.
That’s why choosing the right statin for you is important.
Factors to Consider when Choosing a Statin
There are many important factors to consider when choosing a statin. Some things to discuss with your healthcare provider include:
- What statin intensity do I require?
- How will my body process the statin?
- What statin is the safest?
- Which statin has the fewest side effects?
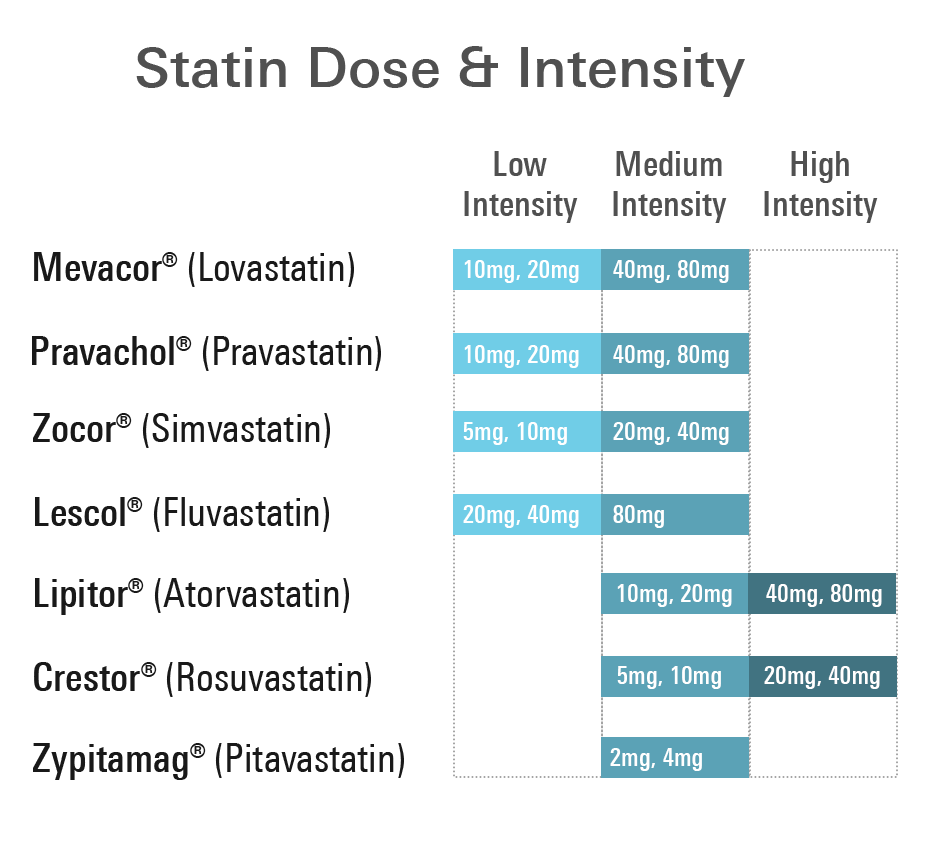
Comparing Statin Dose and Intensity
Statin intensity is a term used in the medical community to describe how much you can expect a statin to lower your bad cholesterol levels. There are low, moderate, and high intensity statins.
- Low intensity statins: Expect less than a 30% decrease in LDL-C or bad cholesterol
- Moderate intensity statin: Expect a 30-49% decrease in LDL-C or bad cholesterol
- High intensity statin: Expect greater than a 50% decrease in LDL-C or bad cholesterol
It’s not all about lowering cholesterol; how to determine the right statin dose for you?
The right statin dose and intensity you require is something you should discuss with your healthcare provider.
For example, if you have previously had a heart attack or stroke it is recommended that you initiate a high-intensity statin, or maximally tolerated statin right away.
If you are diabetic, the more recent blood cholesterol guidelines recommend anyone ages 40 to 75 should be taking a moderate-intensity statin, regardless of your cholesterol levels.
It can depend on quite a few factors. See below for some risk enhancing factors that would suggest you may need to start taking a statin, or a higher intensity statin.
ACC/AHA ASCVD Risk Enhancing Factors:
- Family history of premature cardiovascular disease
- Persistently elevated LDL-C levels ≥ 160 mg/dL
- Metabolic syndrome
- Chronic kidney disease
- Conditions specific to women (e.g. preeclampsia, premature menopause)
- Inflammatory diseases (especially rheumatoid arthritis, psoriasis, HIV)
- Ethnicity (e.g. South Asian ancestry)
- Persistently elevated triglycerides ≥ 175 mg/dL
- Other markers such as: hs-CRP levels ≥ 2.0 mg/L, Lp(a) levels > 50 mg/dL, apo B levels ≥ 130 mg/dL, or ankle-brachial index (ABI) < 0.9
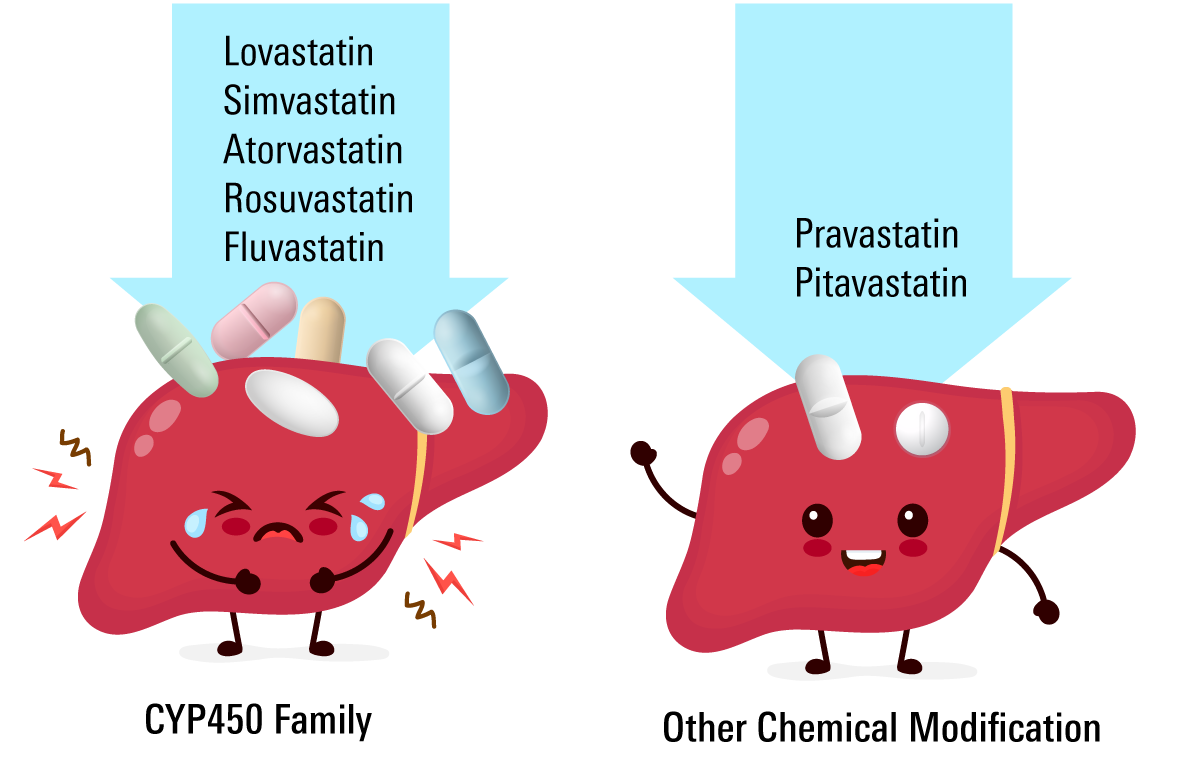
Comparing Statin Risk for Drug Interactions
Some statins have a reduced potential to interact with other medications and food than others. If you are taking multiple medications, or enjoy certain beverages like grapefruit juice, then this is a very important consideration when choosing your statin!
Busy Enzyme Pathways Can Create Unwanted Drug-Interactions
70-80% of medications are metabolized by the same enzyme family called the cytochrome 450 (CYP450) family of enzymes.
When drug-drug and drug-food interactions occur this can lead to:
- Drugs become less active: this means there is less drug than expected in your body
- Drugs become more active: this means there is more drug than expected in your body
- Adverse reactions: too much or too little of a medication can lead to adverse reactions and can be very dangerous in some circumstances
Grapefruit juice is the classic example for statins. Grapefruit juice interacts with the CYP450 family of enzymes. When combined with atorvastatin it can lead to dangerously high levels of atorvastatin in our blood and this can result in adverse effects.
Which statin has the fewest side effects?
Statin side effects is the number one reason that patients claim to stop taking their statin. The most common side effects associated with a statin are:
- Headache
- Diarrhea
- Constipation
- Muscle pain
- Weakness
Statin Side Effects Increase with Dosage
Generally speaking, the higher the dose of statin you take, the higher the chance of side effects. If you experience a statin side effect, be sure to talk to your healthcare provider. More than likely, they will want to lower your dose or switch statins altogether to see how your body responds.
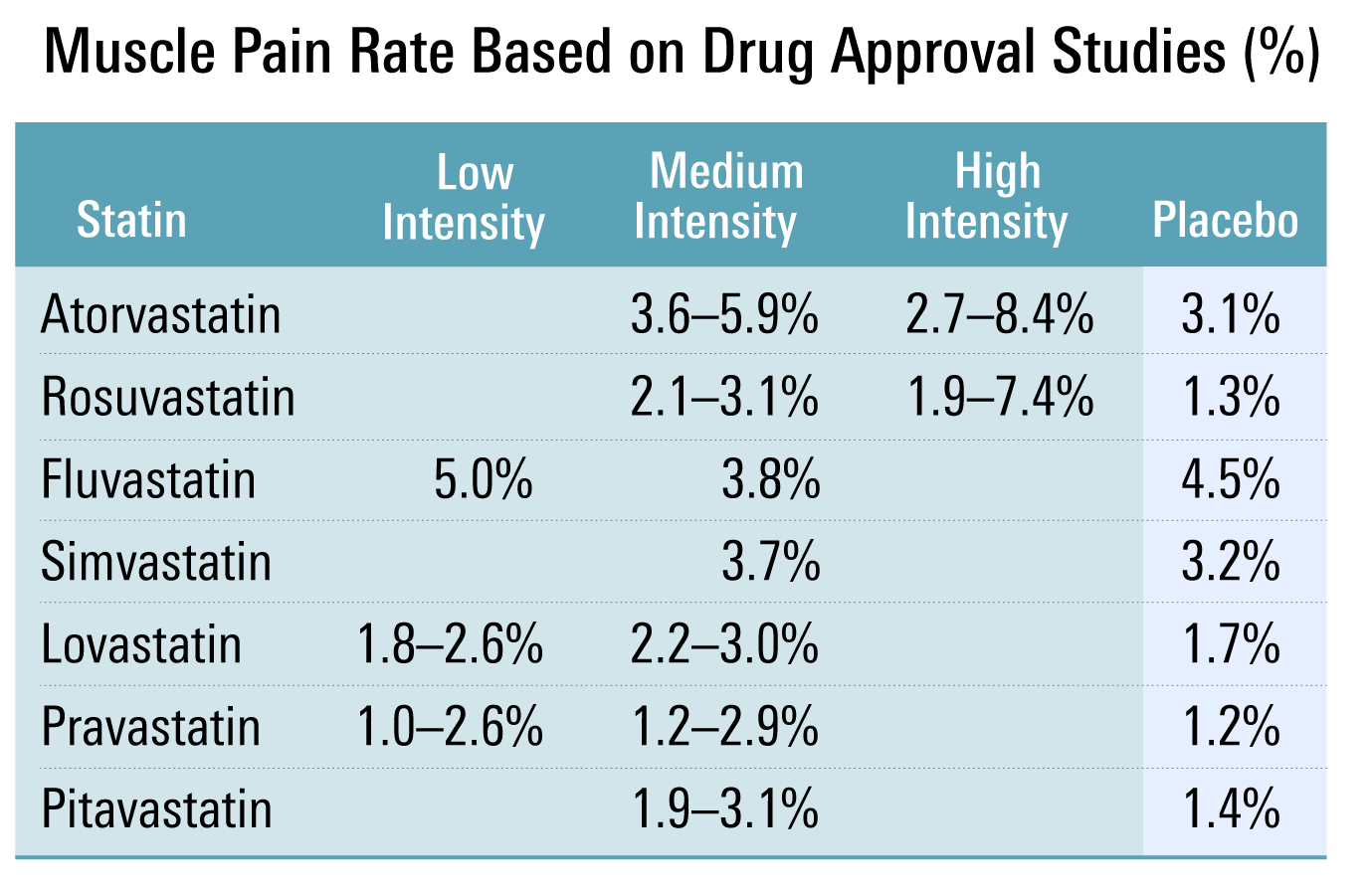
Muscle Pain is the #1 Reason People Stop Taking a Statin
62% of former statin users indicated muscle pain was the reason they stopped taking it. Interestingly, a recent study looked at what is causing this pain, and they found that 90% of cases of muscle pain were due to something called the 'nocebo effect'.
The table below highlights the reported muscle related side effects for each statin.
Choosing a Hydrophilic or Lipophilic Statin
Statins can be categorized as being hydrophilic (water soluble) or lipophilic (fat soluble). Each group has different features which are highlighted below.
From a clinical perspective, both hydrophilic and lipophilic statins have a similar ability to lower the risk of heart attack and stroke.1
Hydrophilic Statin Features
- Water soluble
- Enters cells using transporters
- Specific to the liver
- Cleared from our body by kidneys
- High-dose hydrophilic statins significantly increase the incidence of liver toxicity2
Lipophilic Statin Features
- Fat soluble
- Enters cells passively
- Widely distributed throughout body
- Predominantly processed by CYP450 enzymes (described above)
- Associated with an increased risk of muscle damage (creatine kinase)3
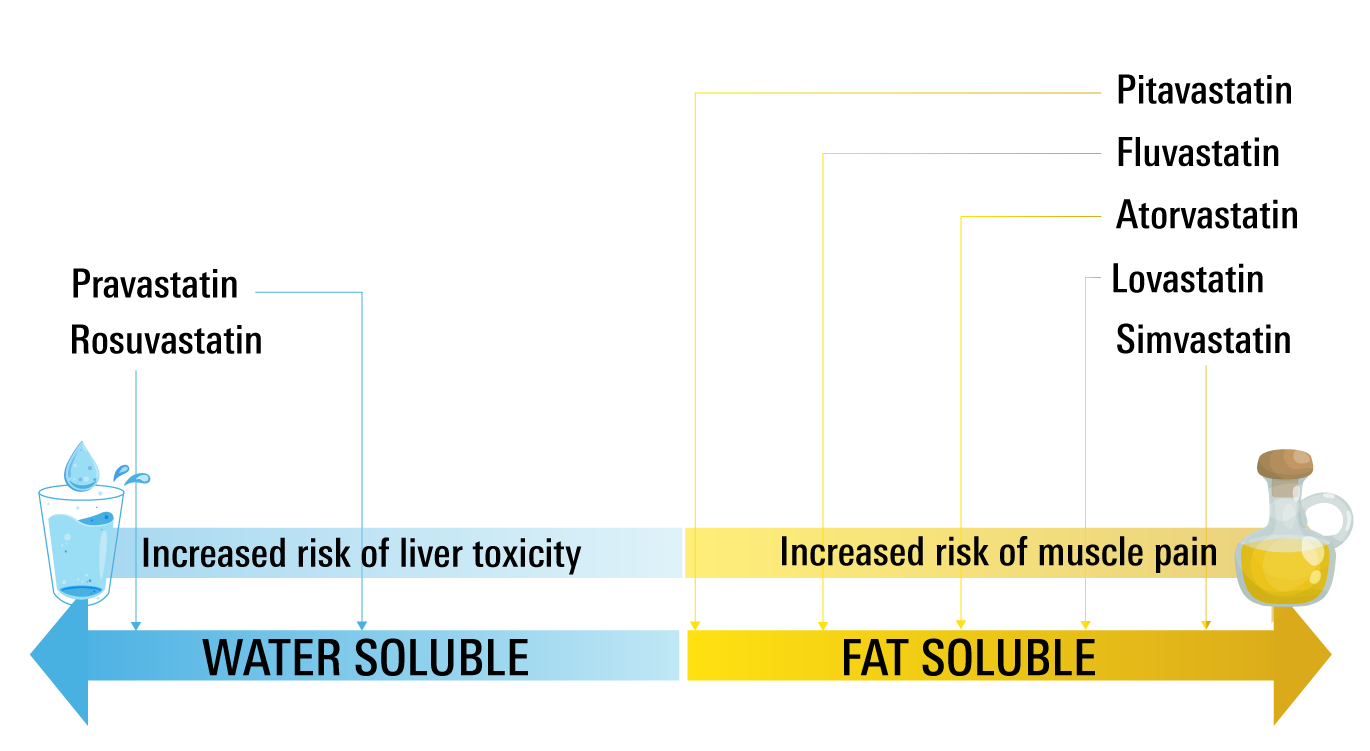
Third-generation statins like pitavastatin shares advantages with statins from both hydrophilic and lipophilic statin families including the ability to reduce bad cholesterol and increase good cholesterol as well as the reduced potential for certain drug-drug interactions.
- Bytyci et al. J Am Coll Cardiol. 2017; 69(11 Supplement):161
- Dale et al. American Journal of Medicine 2007; 120(8): 706-712
- Pastori et al. Digestive and Liver Disease. 2015; 47(1):4-11
Pitavastatin Binds Strongest to the Cholesterol Making Enzyme
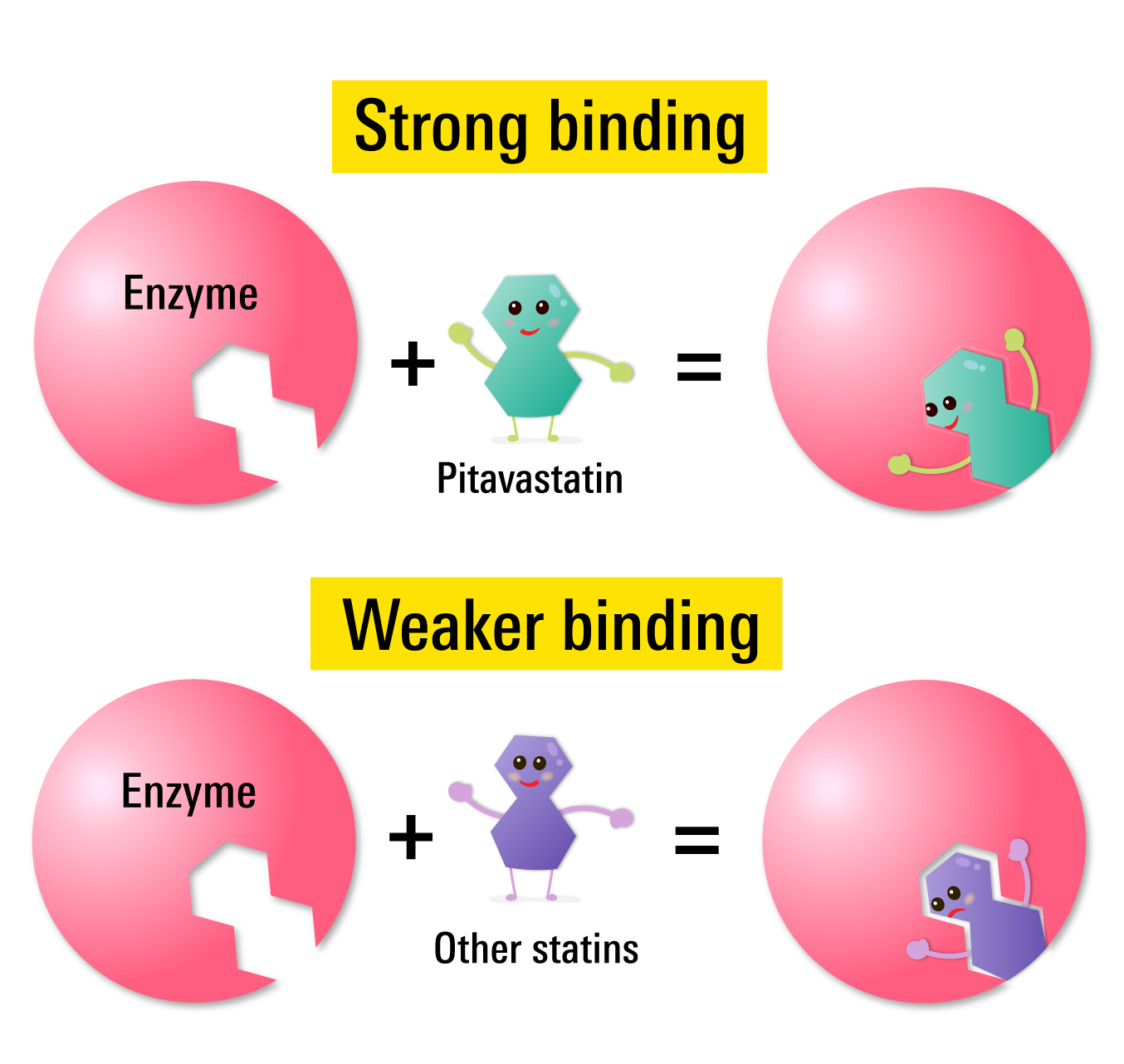
HMG-CoA reductase is one of the enzymes that is responsible for helping to produce cholesterol in our bodies. Statins work by blocking this enzyme.
While each statin binds to this enzyme, each of them bind to the enzyme at different levels (a science term known as their binding affinity).
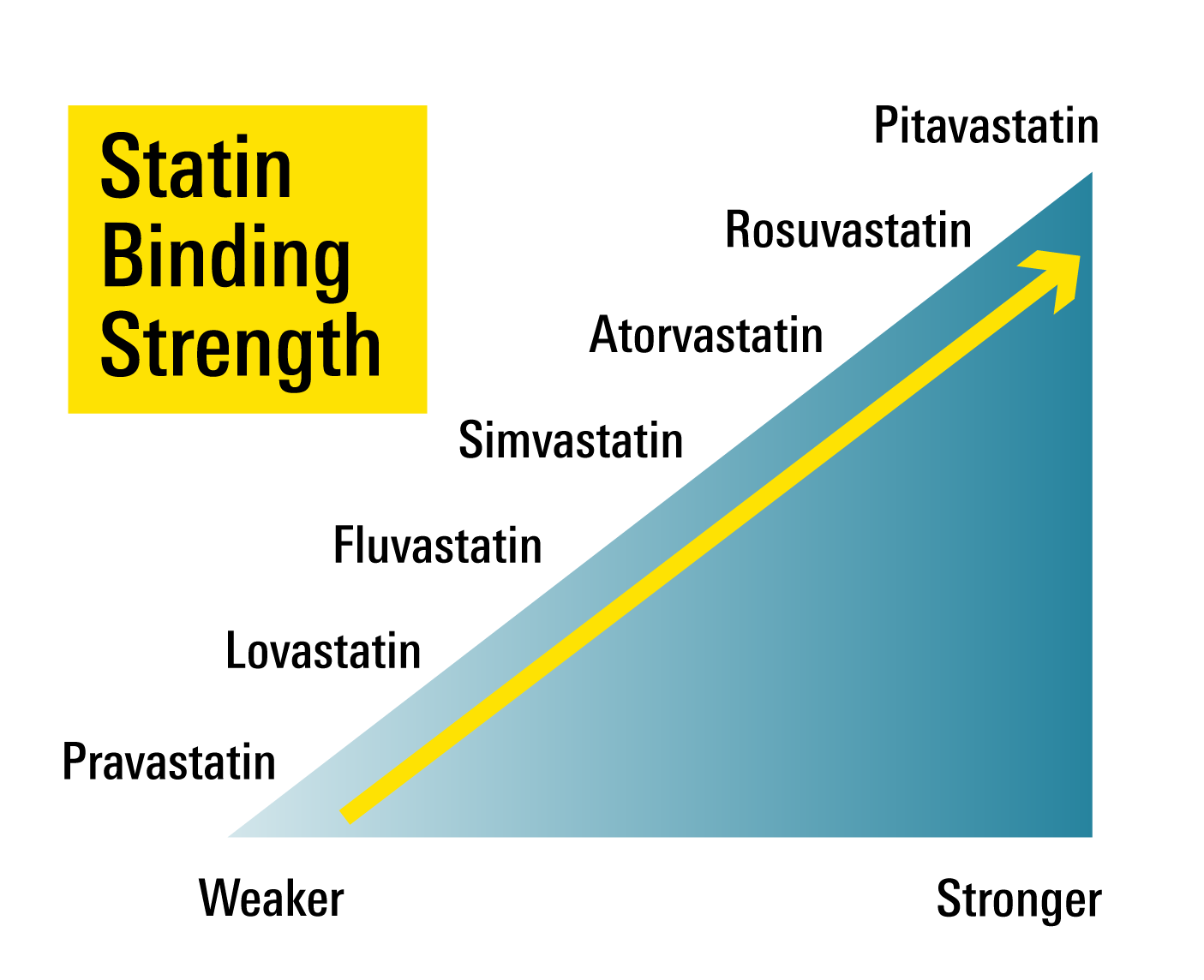 Of the 7 statins available, pitavastatin binds strongest to HMG-CoA reductase, followed by rosuvastatin, then atorvastatin.
Of the 7 statins available, pitavastatin binds strongest to HMG-CoA reductase, followed by rosuvastatin, then atorvastatin.
Pitavastatin's binding ability to cholesterol making enzyme is one of the reasons why you can get away with 2 mg and 4 mg of pitavastatin but need higher doses with most other statins.
When Is the Best Time to Take Your Statin?
There are two important factors to consider about when it's best to take your statin:
- What time of day should I take it?
- Should I take it with food?
What time of day should I take my statin?
Our bodies produce cholesterol primarily at night time. This is the time when the cholesterol making enzyme, HMG-CoA reductase is most active.
Because of this its very important to have our statins actively working in our bodies at night time.
Simvastatin, lovastatin and fluvastatin should all be taken at night time, as if they are taken in the morning, they are not as effective. All other statins, including pravastatin, atorvastatin, rosuvastatin and pitavastatin can be taken at anytime of the day.
Should I take my statin with food?
Previously we talked about statins and their interactions with foods like grapefruit juice. Here we want to discuss very simply, should I take my statin with a meal or not?
Eating a meal with your statin can effect the absorption of the medication for some statins. With lovastatin, you can see an increased absorption of the medication and as a result it is recommended that lovastatin be taken with your evening meal.
On the other hand, eating a meal with pravastatin or atorvastatin reduces the absorption of the medication, by 17% and 9% respectively.
This difference is considered to be minor and as a result the recommendation is that all statins (except for lovastatin) can be taken with or without food.
The Best Time to Take A Statin
| Statin | Time to Take a Statin | With or Without Food |
|---|---|---|
| Lovastatin | Night | With Evening Meal |
| Pravastatin | Anytime | Anytime |
| Simvastatin | Night | Anytime |
| Fluvastatin | Night | Anytime |
| Atorvastatin | Anytime | Anytime |
| Rosuvastatin | Anytime | Anytime |
| Pitavastatin | Anytime | Anytime |