- An arrhythmia refers to abnormal heart rate, being too fast, too slow, or irregular.
- While some arrhythmias are harmless and do not require intervention, others can be life threatening, so all arrhythmias be investigated.
- There are many medications and surgical options available for treatment of arrhythmias that need to be resolved.
Overview
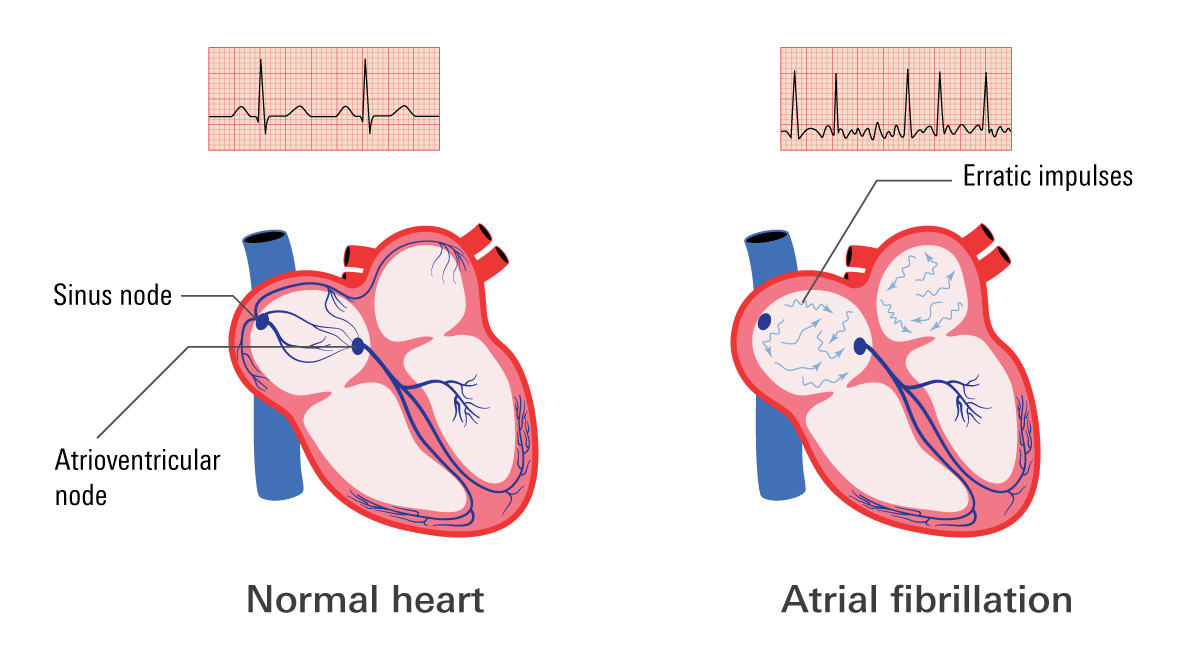
Arrhythmias are irregular heartbeats. An arrhythmia occurs when the heart’s electrical signals get disrupted and causes your heart to beat too fast, too slow, or irregularly. For adults, the heart normally beats (pumps) between 60 and 100 times per minute to circulate blood throughout the body.
If you have arrhythmias, you may experience a feeling of fluttering in the chest, dizziness or shortness of breath. Or you may not have any symptoms.
Many heart arrythmias are harmless. But if they are highly irregular or resulting from a weak or damaged heart they need to be treated with medication or procedures. Left untreated they can lead to stroke, heart failure and other complications.
Prevalence
The prevalence of arrhythmias in the United States is significant. While exact figures can vary based on studies and specific arrhythmia types, it's estimated that around 1.5% to 5% of the general population experiences some form of arrhythmia.
One of the most common arrhythmias is atrial fibrillation (AFib), which affects a substantial portion of the population. The Centers for Disease Control and Prevention (CDC) estimates that approximately 12.1 million people in the U.S. have AFib.
It's important to note that the prevalence of arrhythmias can increase with age and is often associated with other health conditions, such as heart disease, high blood pressure, and certain lifestyle factors.
Symptoms
Arrhythmias, or irregular heartbeats, can manifest in a variety of symptoms. While some individuals may experience no symptoms at all, others may notice the following:
- Heart palpitations: A feeling of fluttering, pounding, or racing in the chest.
- Shortness of breath: Difficulty breathing or a feeling of breathlessness.
- Chest discomfort: Pain or pressure in the chest.
- Fatigue: Excessive tiredness or weakness.
- Dizziness or lightheadedness: A sensation of spinning or feeling faint.
Less common symptoms include:
- Fainting: Loss of consciousness.
- Blackouts: Brief periods of unconsciousness.
- Sweating: Excessive perspiration.
- Nausea or vomiting: Feeling sick to one's stomach.
It's important to note that these symptoms can vary depending on the type of arrhythmia and its severity. If you experience any of these symptoms, it's advisable to consult with a healthcare professional for a proper diagnosis and appropriate treatment.
Types
Some common types of arrhythmias include:
- Tachycardia: a heart rate faster than 100 bpm and/or beats irregularly.
- Bradycardia: a heart rate that’s too slow. Slower than 60 bpm.
- Atrial Fibrillation (Afib)
The most common type of arrhythmia, affecting over 2.5 million Americans. The upper chambers (the atria) of the heart beat so fast they quiver or fibrillate, causing lower chambers (the ventricles) to beat out of sync.
- Ventricular fibrillation (VF)
Tthe lower chambers quiver instead of pumping blood into the body. VF is a life-threatening condition that can lead to cardiac arrest.
Causes
Arrhythmias can be caused by a variety of factors, including:
- Heart conditions: Coronary artery disease, heart failure, or congenital heart defects can disrupt the heart's electrical signals.
- High blood pressure: Elevated blood pressure can put stress on the heart and increase the risk of arrhythmias.
- Electrolyte imbalances: Low levels of potassium, magnesium, or calcium can affect the heart's electrical function.
- Thyroid disorders: Hyperthyroidism (overactive thyroid) or hypothyroidism (underactive thyroid) can influence heart rate.
- Certain medications: Some medications, such as beta-blockers or digitalis, can cause or worsen arrhythmias.
- Stimulants: Excessive caffeine or cocaine use can trigger arrhythmias.
Risk Factors
Several factors can increase your risk of developing arrhythmias:
- Age: The risk of arrhythmias increases as you get older.
- Family history: A family history of arrhythmias can make you more susceptible.
- Health conditions: High blood pressure, heart disease, obesity, kidney disease, chronic obstructive pulmonary disease (COPD), sleep apnea, and viral infections can contribute to arrhythmias.
- Lifestyle factors: Smoking, drug use, excessive alcohol consumption, stress, and anxiety can increase the risk.
It's important to consult with a healthcare professional if you have concerns about your risk factors or are experiencing symptoms of arrhythmias. Early diagnosis and treatment can help manage the condition and prevent complications.
Diagnosis
If you are experiencing symptoms or suspected of having an arrhythmia there are several different diagnostic tests that can be done.
- An electrocardiogram (ECG) is the most common test. It captures a short record of the electrical activity of your heart. If the abnormal rate isn’t always present, the ECG may not catch the abnormalities.
- Holter monitors are portable, 24-hour ECGs. They help detect arrhythmias that may come and go throughout the day.
- Echocardiogram is an ultrasound that provides a picture of the size, structure, and motion of your heart.
If your doctor doesn’t find an arrhythmia with the above tests, they may order a test that triggers the arrhythmia.
- Stress test is a test that monitors your heart rate during exercise. You’re asked walk on a treadmill or ride a stationary bicycle while your heart is monitored.
- Tilt table test—if you have fainting spells, your doctor may order a tilt table test. You lie flat on the table, then table will tilt from horizontal position to vertical position as if you are standing up. Your heart rate and blood pressure are measured while you’re on the table.
- Electrophysiological testing and mapping (EP)—catheters with electrodes on the tip were inserted through the blood vessels to the heart. The electrodes can map the electrical signals through the heart. It can trigger hidden arrhythmias.
Treatment
The treatment of arrhythmias depends on the type, severity, underlying cause of the condition. Your doctor typically recommends medication along with lifestyle changes. If they don’t treat your condition adequately, you may need a procedure or a device.
Procedures and devices
- Cardioversion: a procedure that uses electric shock to restore a normal heart rhythm.
- Catheter ablation: a procedure using radiofrequency (RF) or laser light to create a scar on the heart. The star prevents abnormal electrical signals from causing arrhythmias.
- Implantable devices: a pacemaker or a defibrillator can help regulate the heart's rhythm and prevent dangerous arrhythmias.
Medication options
Antiarrhythmics
Antiarrhythmics work by blocking electrical channels to slow down your heart rate and allow it to beat at a regular rhythm. Depending on your specific condition there are several different antiarrhythmics that may be best suited for you.
Examples of antiarrythmics include: amiodarone, flecainide, propafenone, sotalol, diltiazem
Beta-blockers
Beta blockers work by reducing the release of the hormones adrenaline and noradrenaline. Your body uses adrenaline and noradrenaline to activate your “fight-or-flight” response, which causes rapid heartbeat, high blood pressure, excessive sweating, anxiety, and heart palpitations. Beta-blockers work by slowing the heart rate and reducing the workload on the heart.
Examples of beta-blockers for arrythmias include: metoprolol, propranolol, carvedilol, bisoprolol, atenolol.
Blood thinners (anticoagulants)
Anticoagulants are often used to treat arrhythmias that increase the risk of blood clots, such as atrial fibrillation. When a blood clot forms in the heart or brain, it can lead to an event like a heart attack or stroke. By reducing the levels of clotting factors in your blood, blood thinners decrease the chance of these events occurring as a result of your arrhythmia.
Examples of anticoagulants for arrythmias include: warfarin, dabigatran, rivaroxaban, apixaban.
Calcium channel blockers (CCBs)
Calcium channel blockers decrease the amount of calcium that enter the heart and blood vessel walls. This relaxes the blood vessels and heart, resulting in improved blood pressure and a more controlled heart rate.
Examples of CCBs for arrythmias include: verapamil, diltiazem, nifedipine.
Digoxin
Digoxin works by slowing down the electrical impulses in the heart to control the heart rhythm. This puts less pressure on your heart and increases the amount of blood your heart can fill with and then pump out with each beat.
Related Topics
Five Most Common Arrhythmias
In typical adults, the heart beats at a rate of 60–100 beats per minute (bpm). Heart rhythm is a result of specific coordination of electrical signals throughout the heart. Sometimes there are problems within the system, and the rhythm loses its regularity.
Read more