- Benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland, commonly affecting older men.
- Common symptoms include frequent urination, urgency, weak urine stream, difficulty starting urination, and incomplete bladder emptying.
- Age, hormonal changes, genetics, obesity, sedentary lifestyle, and certain medical conditions like diabetes and heart disease.
- Treatment options include watchful waiting, medications (alpha-blockers, 5-alpha-reductase inhibitors), minimally invasive procedures, and surgical interventions.
- While BPH cannot be entirely prevented, maintaining a healthy lifestyle and balanced diet may help reduce the risk or manage symptoms.
Overview
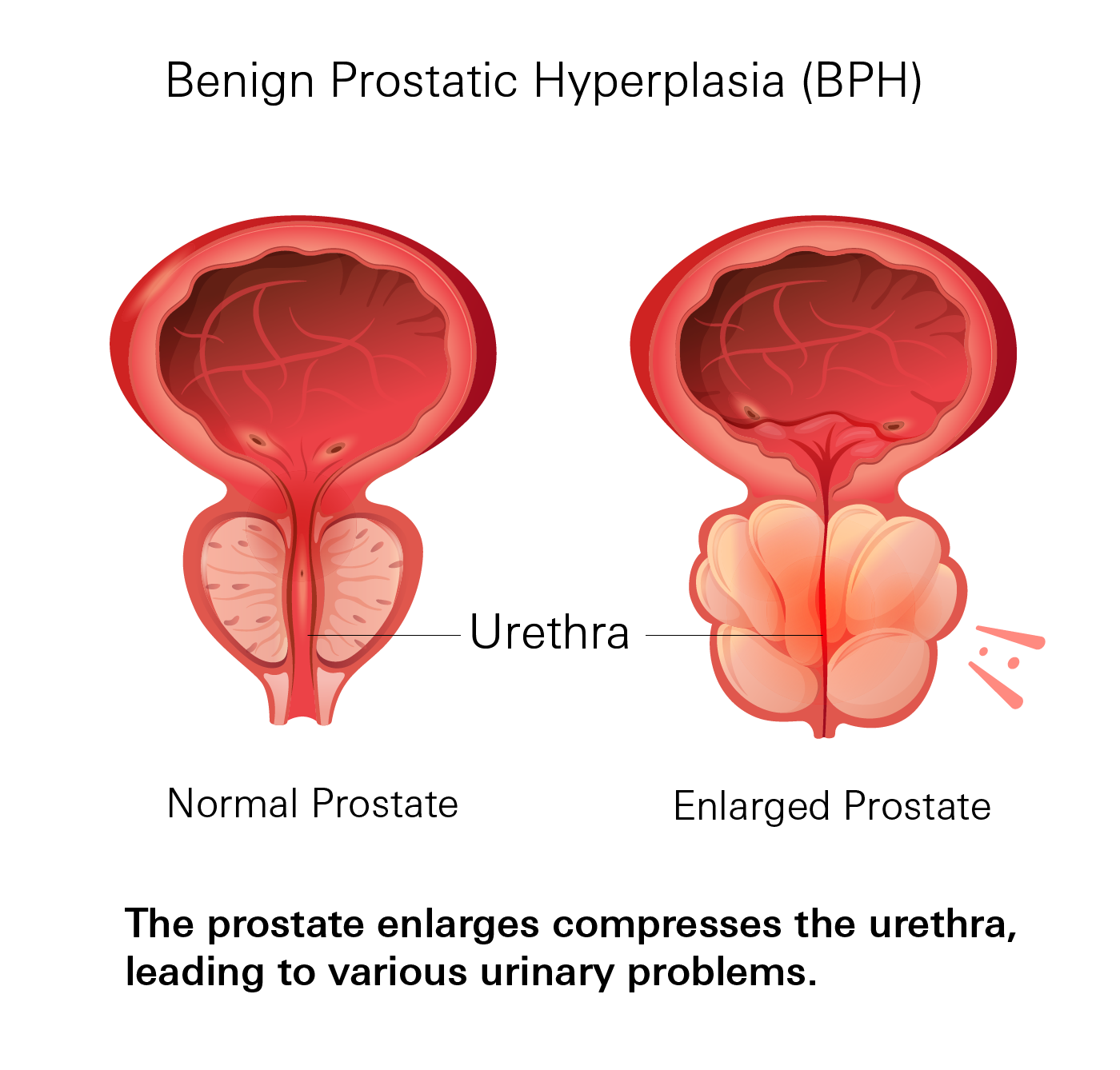
BPH, also known as prostate gland enlargement, is a non-cancerous condition affecting many older men. It occurs when the prostate gland, located just below the bladder, grows abnormally. As the prostate enlarges, it can compress the urethra, the tube that carries urine out of the body, leading to various urinary problems.
While the exact cause of BPH is not fully understood, age and hormonal changes are believed to play significant roles. As men age, levels of dihydrotestosterone (DHT), a hormone that promotes prostate growth, increase. This hormonal imbalance can stimulate excessive prostate cell growth.
If left untreated, BPH can lead to complications such as urinary tract infections, bladder stones, and even kidney damage. Therefore, it's essential to seek medical attention if you experience symptoms associated with this condition.
Prevalence
BPH is a highly prevalent condition, particularly among older men. The risk of developing BPH increases significantly with age.
According to the American Urological Association (AUA), approximately half of men between the ages of 51 and 60 exhibit signs of BPH, as evidenced by histological examination of prostate tissue. This percentage rises to around 90% by the time men reach 80 years old. It's important to note that while histological evidence indicates the presence of BPH, not all individuals with BPH will experience noticeable symptoms.
If you have any concerns regarding BPH or are currently experiencing symptoms, it is strongly recommended to seek guidance from a healthcare professional for an accurate diagnosis and appropriate management.
Symptoms
BPH can cause a range of urinary symptoms that may vary in severity from person to person. Common symptoms include:
- Urinary frequency: Needing to urinate more often than usual, especially at night (nocturia).
- Urgency: A sudden, strong urge to urinate that's difficult to delay.
- Weak urine stream: A reduced force of the urine stream.
- Hesitancy: Difficulty starting or maintaining the flow of urine.
- Intermittent stream: A urine stream that starts and stops.
- Incomplete emptying: Feeling like your bladder isn't fully emptied after urinating.
- Urinary retention: Difficulty emptying your bladder completely.
- Dribbling: Leaking urine after urination.
- Urinary tract infections (UTIs): An increased risk of UTIs due to incomplete bladder emptying.
If left untreated, severe BPH can lead to complications such as bladder stones, urinary tract infections, bladder damage, or kidney problems. It's crucial to seek medical attention if you experience any of these symptoms.
While these symptoms are commonly associated with BPH, they can also be indicative of other urological conditions. If you notice any of these symptoms, it's important to consult with your doctor for a proper diagnosis and appropriate treatment.
Causes
The exact cause of BPH is not fully understood, but several theories and factors may contribute to its development. Some possible causes and factors include:
- Age: The risk of developing BPH increases with age. It is most commonly seen in men over the age of 50 and becomes more prevalent as men get older. Age-related changes in the prostate gland and hormonal balance play significant roles in its development.
- Hormonal Changes: BPH is associated with changes in hormonal levels, particularly an increase in dihydrotestosterone (DHT). DHT is derived from testosterone and plays a role in the growth and enlargement of the prostate gland.
- Genetics: There may be a genetic predisposition to BPH, as it tends to run in families. If a man’s father or brother has had this condition, he may be at a higher risk of developing it himself.
- Obesity: Being overweight or obese has been associated with an increased risk of developing BPH. Excess weight and adipose tissue can lead to hormonal imbalances and inflammation, which may contribute to the development of BPH.
- Lifestyle Factors: Certain lifestyle choices and habits have been linked to an increased risk of BPH. These include a sedentary lifestyle, lack of physical activity, and a diet high in fat and low in fruits and vegetables.
- Other Medical Conditions: Certain medical conditions, such as diabetes and heart disease, have been associated with an increased risk of developing BPH. However, the exact mechanisms underlying these relationships are not yet fully understood.
It's important to note that while these factors can increase the likelihood of developing BPH, they don't guarantee it. Some individuals may develop BPH despite not having any of these risk factors, and others may have multiple risk factors without developing the condition.
Diagnosis
Diagnosing BPH typically involves a multi-step approach to assess your symptoms, rule out other causes, and determine the severity of the condition. Here's what you can expect:
- Medical History: Your doctor will discuss your symptoms in detail, including their duration, severity, and any history of urinary tract infections or other medical conditions. They will also inquire about medications you're taking, as some can affect urination.
- Physical Exam: A digital rectal exam (DRE) allows your doctor to feel the size, shape, and consistency of your prostate through the rectum. This helps detect any abnormalities that might indicate BPH or other prostate-related conditions.
- Lab Tests:
- Prostate-Specific Antigen (PSA) Blood Test: PSA is a protein produced by the prostate. While elevated PSA levels can occur with BPH, they can also point towards prostate cancer. This test helps assess your prostate health, but its results alone don't diagnose BPH.
- Urine Test: A urine sample can identify signs of infection or other issues that might contribute to your urinary symptoms.
- Urinary Flow Tests: These tests measure the strength and pattern of your urine flow. They help assess the severity of any blockage and whether your condition is improving or worsening over time.
- Post-void Residual Measurement: This test determines how much urine remains in your bladder after urination. It can be done with ultrasound or a catheter to check for incomplete bladder emptying.
- Imaging Studies: In some cases, additional imaging might be needed. An ultrasound can reveal the prostate's size and structure. In some instances, cystoscopy (a visual examination of the bladder) or urodynamic studies (evaluating bladder function) might be necessary.
The specific tests used will depend on your individual situation and your doctor's judgment. Ultimately, the goal of these diagnostic procedures is to confirm the presence and severity of BPH while ruling out other potential causes like prostate cancer.
Treatment
The best treatment approach for BPH depends on the severity of your symptoms, your overall health, and your personal preferences. Here are some common options:
Non-Surgical Treatments
- Watchful Waiting: For mild BPH with minimal symptoms, your doctor may recommend monitoring your condition without immediate intervention. Lifestyle changes and self-care measures can help manage symptoms.
- Medications
- Alpha-blockers (Terazosin, Tamsulosin): First-line treatment for moderate to severe symptoms. Relax the muscles of the prostate and bladder neck, improving urine flow. May be used alone or in combination with 5-alpha-reductase inhibitors.
- 5-alpha-reductase inhibitors (Finasteride): Shrink the prostate by blocking the conversion of testosterone to DHT. Prescribed for significantly enlarged prostates
- Combination therapy: Using both alpha-blockers and 5-alpha-reductase inhibitors for severe BPH.
- Other medications: Drugs like phosphodiesterase-5 inhibitors can address specific symptoms.
Minimally Invasive Procedures
- Transurethral Microwave Therapy (TUMT): Uses heat to shrink the prostate tissue.
- Laser Therapy: Techniques like HoLEP and Greenlight laser therapy use laser energy to remove or reduce prostate tissue.
Surgical Interventions
In cases of severe BPH or when other treatments have been ineffective, surgical procedures may be considered. These interventions involve removing or reducing the size of the prostate gland. Common surgical procedures for BPH include:
- Transurethral Resection of the Prostate (TURP): Uses an instrument inserted through the urethra to remove excess prostate tissue.
- Transurethral Incision of the Prostate (TUIP): Creates small incisions in the prostate to improve urine flow.
- Open Prostatectomy: For very large prostates, this involves open surgery to remove the enlarged tissue.
The choice of treatment will depend on your individual circumstances and your doctor's recommendations. It's essential to discuss the benefits, risks, and potential outcomes of each option to make an informed decision.
Prevention
Unfortunately, there are no known ways to entirely prevent the development of benign prostatic hyperplasia (BPH). This condition is primarily age-related and influenced by hormonal changes and other factors.
- Maintain a Healthy Lifestyle: Engage in regular physical activity and maintain a healthy weight. Regular exercise has been associated with a lower risk of BPH and can help manage symptoms.
- Balanced Diet: Consume a nutritious diet rich in fruits, vegetables, whole grains, and lean proteins. A balanced diet can support overall health and may help reduce the risk of BPH.
While these measures cannot guarantee prevention, they can contribute to better prostate health and overall well-being. If you have concerns about BPH or are experiencing symptoms, it is advisable to consult with a healthcare professional for personalized advice and management strategies.
Related Topics
The Anatomy of The Prostate
The prostate is a part of the male reproductive system which also includes the penis, testicles, and seminal vesicles. Located just below the bladder and in front of the rectum, the prostate is a small gland, roughly the size and shape of a walnut and weighs approximately 30 grams or 1 ounce.
Read moreWhat is Benign Prostatic Hyperplasia?
Benign prostatic hyperplasia, often referred to as BPH, is the enlargement of the prostate that is usually benign (non-cancerous) and is common in men as they age. When your prostate becomes enlarged, it usually interferes with one’s ability to urinate due to the fact that the prostate completely surrounds your urethra—the tube that carries urine from your bladder to outside of your body.
Read moreBenign Prostatic Hyperplasia Medications
This drug class of medications (selective and non-selective) is considered first-line for individuals with moderate to severe symptoms of BPH and may be used alone or in combination with another drug class called 5 alpha-reductase inhibitors.
Read more