- Celiac disease is an autoimmune condition triggered by consuming gluten, a protein found in wheat, barley, and rye.
- It damages the lining of the small intestine, affecting nutrient absorption.
- Symptoms include diarrhea, fatigue, weight loss, and bloating.
- Untreated celiac disease can lead to long-term complications such as malnutrition, osteoporosis, infertility, skin rashes, and an increased risk of certain cancers.
- Managing celiac disease involves following a strict gluten-free diet.
Overview
Celiac disease, also known as celiac sprue or gluten-sensitive enteropathy, is an autoimmune condition that primarily affects the small intestine. The disease is triggered by the consumption of gluten, a protein found in wheat, barley, and rye. When someone with celiac disease ingests gluten, their immune system attacks the small intestine, damaging the lining of the intestinal wall. As a result, the absorption of nutrients from food is impaired, leading to various health issues.
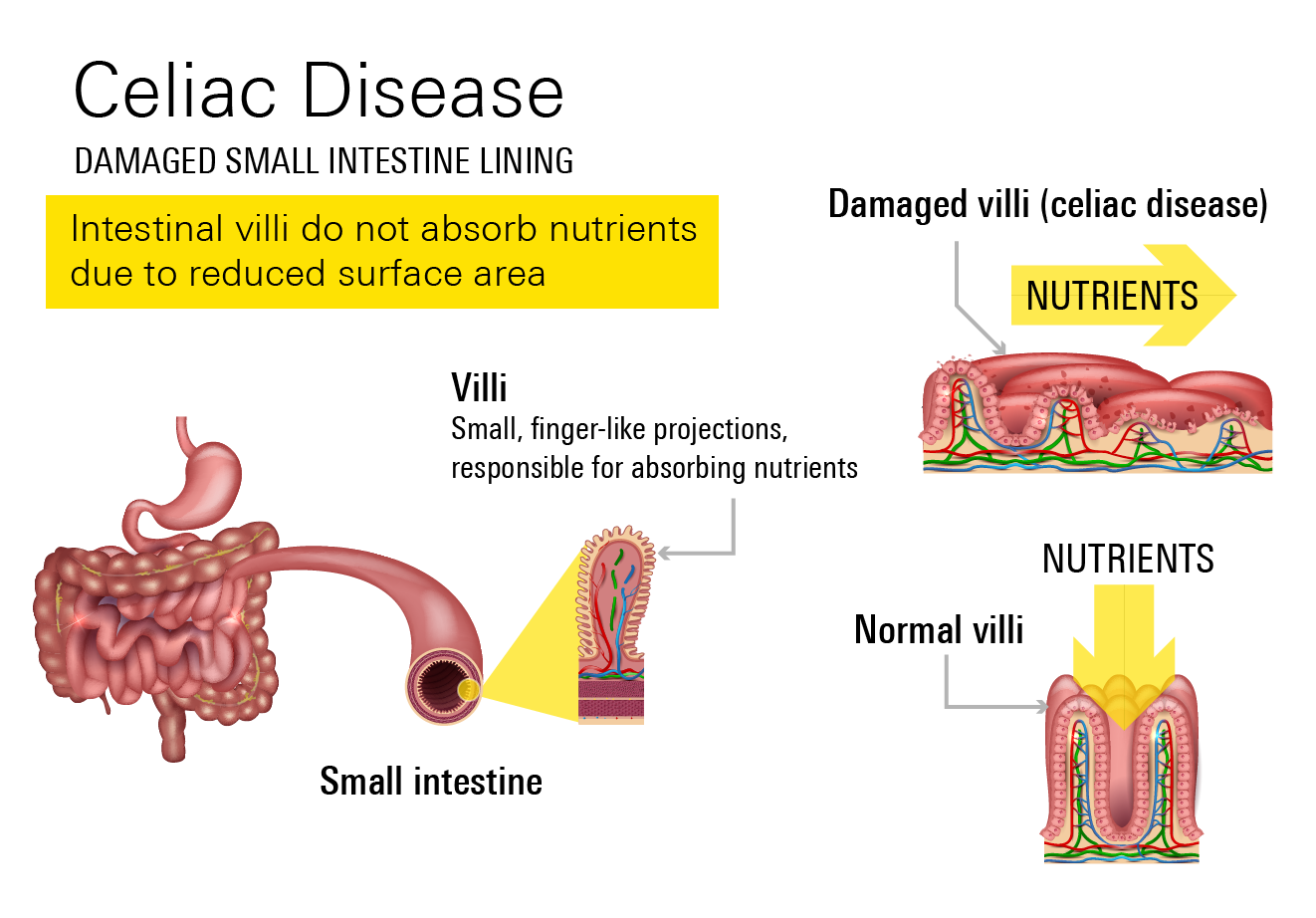
Since the intestinal lining has been damaged, it’s more difficult for nutrients from meals to be absorbed, resulting in malnourishment. While the specific etiology of celiac disease is not entirely understood, it's thought to be a mix of hereditary and environmental factors.
Celiac disease can be managed by a strict gluten-free diet. To avoid any potential long-term problems, monitoring by your doctor is essential.
Prevalence
Celiac disease affects approximately 1% of the population in the United States, which translates to roughly 3 million Americans. However, many cases of celiac disease go undiagnosed or misdiagnosed, which means the actual number of individuals affected may be higher.
Symptoms
Symptoms of celiac disease are the specific signs and manifestations that individuals with the condition experience. These symptoms can vary in severity and may differ among individuals. Common symptoms of celiac disease include:
- Digestive problems: These can include recurring abdominal pain, bloating, gas, diarrhea, constipation, vomiting, and/or nausea.
- Weight changes: Unexplained weight loss or difficulty gaining weight despite adequate food intake may be observed.
- Fatigue and/or weakness: Persistent fatigue, feeling tired, and/or experiencing general weakness.
- Nutritional deficiencies: Celiac disease can lead to deficiencies in essential nutrients including iron, calcium, vitamin D, and vitamin B12. This may result in anemia, osteoporosis, and/or other vitamin and mineral deficiencies.
- Issues with your skin: Some may experience dermatitis herpetiformis, which is a skin rash described as itchy, blistering lesions.
- Joint and bone pain: Celiac disease can cause joint pain, muscle cramps, and/or bone pain, which may be related to calcium and vitamin D deficiencies.
- Delayed growth and puberty: In children, celiac disease can impair growth and delay the onset of puberty.
- Neurological Symptoms: Some may experience neurological symptoms such as headaches, migraines, peripheral neuropathy, or problems with balance and coordination.
Complications
Complications of celiac disease are long-term consequences that can arise if the condition is left untreated or poorly managed.
When individuals with celiac disease continue to consume gluten, it triggers an immune response that damages the lining of their small intestine. Over time, this damage and inflammation can affect multiple systems and result in the following issues:
- Malnutrition: Damage to the small intestine hampers the absorption of essential nutrients like vitamins, minerals, and fats. This can lead to deficiencies in iron, calcium, vitamin D, vitamin B12, and others, causing problems such as anemia, osteoporosis, and nutritional deficiencies.
- Osteoporosis and bone fractures: Malabsorption of calcium and vitamin D can result in weakened and brittle bones, leading to osteoporosis and an increased risk of bone fractures, especially in the wrists, hips, and spine.
- Infertility and pregnancy complications: Both male and female fertility can be affected by celiac disease. Untreated celiac disease may make it more challenging for women to conceive and increase the likelihood of miscarriage. It can also raise the risk of complications during pregnancy, including preterm birth, low birth weight, and developmental issues in infants.
- Dermatitis Herpetiformis: Celiac disease is associated with a skin condition called dermatitis herpetiformis. It manifests as itchy and uncomfortable skin rashes, typically found on the back, buttocks, scalp, and elbows. Both celiac disease and dermatitis herpetiformis require strict adherence to a gluten-free diet since both conditions are triggered by an immune response to gluten.
- Increased risk of certain cancers: People with celiac disease have a slightly higher risk of developing certain gastrointestinal cancers, such as lymphoma and small intestine adenocarcinoma. However, following a strict gluten-free diet significantly reduces this risk.
These serious complications can be avoided or minimized by diligently following a gluten-free diet and receiving regular medical monitoring. Unfortunately, when celiac disease is not effectively treated or managed, these complications are more likely to arise.
Causes
The exact cause of celiac disease is not known for certain, but it is believed to be a combination of genetic, environmental, and immunological factors.
Genetics
Celiac disease has a strong genetic component. Certain genes, like the human leukocyte antigen (HLA) genes, have a significant role in its development. Gene mutations, such as HLA-DQ2 or HLA-DQ8, increase the risk of celiac disease. Having specific variants of HLA genes, like HLA-DQ2 and HLA-DQ8, raises the likelihood of developing the condition.
Environmental trigger
The primary trigger for celiac disease is consuming gluten. If you have a genetic predisposition to the disease and consume gluten, it triggers an abnormal immune response that damages the lining of your small intestine.
Autoimmune response
Celiac disease is considered an autoimmune disorder because the immune system mistakenly attacks the body's own tissues. In the case of celiac disease, the immune system reacts to gluten as if it were harmful, causing inflammation and damage to the small intestine.
Other factors
Additional factors, such as the timing of gluten introduction during infancy, gastrointestinal infections, and other environmental triggers, may contribute to the development of celiac disease. However, further research is needed to fully understand their specific roles. Although the exact cause of celiac disease is unknown, it's thought to be a result of a combination of genetic, environmental, and immunological factors.
Risk Factors
There are a few risk factors affiliated with the development of this condition. These factors can increase your likelihood of developing this condition.
- Genetic predisposition: Having certain genes, particularly human leukocyte antigen (HLA) genes, increases your risk.
- Family history: Having a close relative, such as a parent and/or sibling, with celiac disease increases your risk.
- Age: Celiac disease can manifest at any age, but there are 2 distinct age-related patterns. The first pattern occurs in early childhood, often after gluten is introduced into the diet. The second pattern occurs in adulthood, with the onset of symptoms typically between the ages of 30 and 40. However, it’s important to note that this medical condition can develop at any age.
- Gender: Females have a slightly higher chance of developing celiac disease compared to males, although the reasons behind this difference are not completely understood.
- Early introduction to gluten: Some studies suggest that introducing gluten to an infant's diet too early, such as before 4 months of age, or too late, such as after 7 months of age, may increase the risk of developing this condition.
- Other medical conditions: Celiac disease is more commonly found in those with other autoimmune disorders, including type 1 diabetes, Hashimoto's thyroiditis, Graves' disease, and dermatitis herpetiformis.
Particular medical conditions, such as Down syndrome, Turner syndrome, and Williams syndrome are associated with an increased risk of developing celiac disease.
It's essential to remember that while these risk factors raise the possibility that someone may acquire celiac disease, they don't guarantee that they will. Without these risk factors, celiac disease is still possible to develop, and not everyone who has these risk factors will also develop it.
Diagnosis
Blood tests, physical exams, and, at times, intestinal biopsies are often used to diagnose this medical condition. Some diagnostic methods that are used include the following:
- Medical evaluation: Your healthcare provider will begin by reviewing your medical history and conducting a physical exam. They will inquire about symptoms, family history, and any previous testing or dietary changes.
- Blood tests: Blood tests are performed to check for specific antibodies associated with celiac disease. The most common blood test is the serology test, which measures the levels of certain antibodies. Elevated levels of these antibodies may suggest an immune reaction to gluten.
- Genetic testing: Genetic testing may be conducted to identify the presence of specific HLA genes associated with celiac disease, including HLA-DQ2 and HLA-DQ8. However, since these genes are found in a significant portion of the population without celiac disease, their absence does not rule out the possibility of developing this condition.
- Intestinal Biopsy: If your blood tests suggest a high likelihood of celiac disease, an intestinal biopsy may be performed to confirm the diagnosis. During an endoscopy procedure, a small tissue sample, otherwise known as a biopsy, is taken from the lining of your small intestine. The sample is then examined under a microscope to assess the presence of characteristic changes associated with celiac disease.
Treatment
Commitment to a strict gluten-free diet is the main and best therapy for celiac disease. Since even trace levels of gluten can provoke an immune response and affect your small intestine, it's necessary to completely forego all meals and products that contain gluten. A lifetime dedication, the gluten-free diet necessitates careful consideration of food selection and ingredient lists.
Gluten-free diet
This entails avoiding any gluten-containing foods, such as wheat, barley, rye, and products made from those grains. Bread, pasta, cereal, baked products, and many processed meals are everyday items to avoid. Because gluten may be present in unexpected products like sauces, spices, and even certain drugs, it's crucial to read food labels carefully.Nutritional management
Working with a medical professional or qualified dietitian to ensure a well-balanced and nutrient-rich gluten-free diet is essential if you have celiac disease since it can result in nutritional shortages. It may be advised to take nutritional supplements, particularly to correct deficiencies such as iron, calcium, vitamin D, and vitamin B12.Education and support
Learning about the gluten-free diet and how to spot inadvertent sources of gluten are vital. Attending support groups can provide you with access to experts with personal experience of celiac disease who can offer you emotional support.Monitoring and follow-Up
It's necessary to have regular check-ups by a medical expert to monitor your small intestine's recovery, control symptoms, and maintain adherence to the gluten-free diet.
Prevention
Currently, there is no known way to prevent the development of celiac disease. This medical condition is primarily influenced by genetic factors, and those with a genetic predisposition may develop this condition at some point in their lives.
However, by focusing on early diagnosis, those with celiac disease can effectively manage this condition and prevent complications. Adhering strictly to a gluten-free diet is the key to controlling celiac disease and minimizing damage to your small intestine. Regular monitoring and follow-up with your doctor can help assess the response to your diet and ensure optimal management.
Related Topics
Gluten-Free Living: Insights into Celiac Disease
In celiac disease, these villi become damaged and flattened, reducing their ability to absorb nutrients effectively. This damage, or atrophy, can lead to malabsorption, where the body struggles to absorb vital nutrients
Read more