- Crohn's disease is chronic inflammatory bowel disease, causing inflammation and damage to the digestive tract.
- Common symptoms include abdominal pain, diarrhea, fatigue, weight loss, rectal bleeding, joint pain, skin issues, and eye inflammation.
- The exact cause of Crohn's disease is unknown, but a combinations of genetic, environmental, and immune factors increase the risk of developing the disease.
- There is no cure for the disease, and treatment aims to control symptoms, reduce inflammation, prevent complications, and improve the quality of life.
- Treatment options include medications, nutrition therapy, surgery, lifestyle modifications, and symptom management.
Overview
Crohn's disease is a chronic inflammatory bowel disease (IBD) that primarily affects the gastrointestinal (GI) tract. First described in 1932 by Dr. Burrill B. Crohn, this condition is characterized by inflammation and damage to various parts of the digestive system.
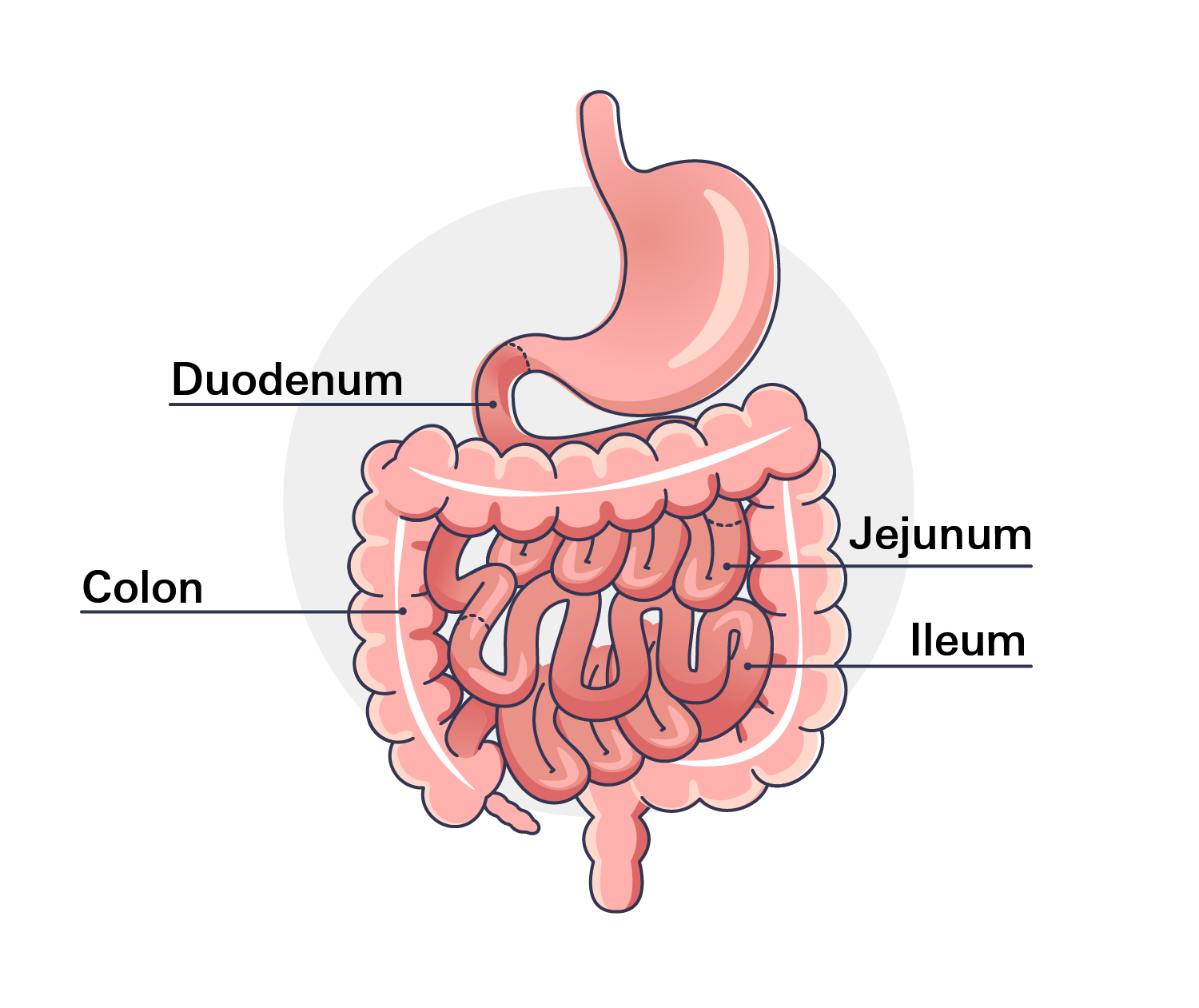
While Crohn's disease can occur anywhere along the GI tract, from the mouth to the anus, it most commonly affects the ileum (the end of the small intestine) and the colon (the beginning of the large intestine). This inflammation can lead to a range of symptoms, including abdominal pain, diarrhea, fatigue, and weight loss.
Crohn's is also classified as an autoimmune disorder. In individuals with this condition, the immune system mistakenly attacks the body's own tissues, causing chronic inflammation and damage.
Common Types of Crohn's Disease
- Ileocolitis: This is the most common type, where inflammation occurs in the ileum (the end of the small intestine) and may extend to the colon.
- Ileitis: In this type, only the ileum is affected.
- Jejunoileitis: This type involves inflammation in the jejunum (the upper part of the small intestine) and the ileum.
- Gastroduodenal Crohn's disease: In this rare type, the stomach and duodenum (the beginning of the small intestine) are affected.
- Crohn's (granulomatous) colitis: This type is limited to the colon.
Prevalence
Crohn's disease is a relatively common. While prevalence rates vary globally, it is more commonly found in developed countries, particularly in North America and Western Europe.
In the United States, approximately 1 to 1.3 million Americans were affected by Crohn's disease as of 2021, and in Europe, the prevalence ranged from 1 to 10 cases per 100,000 people. Globally, Crohn's disease was estimated to affect between 0.1% and 0.5% of the population.
Symptoms
Crohn's disease can cause a wide range of signs and symptoms, which can vary in severity and may come and go over time. The most common signs and symptoms of Crohn’s disease include:
- Abdominal pain and cramping: Persistent pain in the abdomen, often in the lower right or left quadrant.
- Diarrhea: Frequent loose stools, which may be accompanied by urgency or incontinence.
- Fatigue: Feeling tired or weak due to inflammation and nutrient deficiencies.
- Weight loss:: Unintentional weight loss caused by decreased appetite, malabsorption, and increased energy expenditure.
- Fever: Low-grade fever during flare-ups, indicating inflammation in the body.
- Rectal bleeding: Blood in the stool due to inflammation and ulceration in the gastrointestinal tract.
- Joint pain and swelling: Inflammation can affect joints, causing pain and swelling.
- Skin problems: Rashes, ulcers, or sores on the skin.
- Eye inflammation: Redness, pain, or sensitivity to light in the eyes.
- Perianal symptoms: Abscesses, fistulas, or skin tags around the anus..
It's important to know that not all cases of individuals with Crohn's disease will experience all these symptoms, and the severity can vary significantly from person to person. Additionally, Crohn's disease can sometimes be mistaken for other gastrointestinal disorders; therefore, a proper medical evaluation, including imaging and endoscopic procedures, is essential for accurate diagnosis and appropriate treatment.
Causes
The exact cause of Crohn's disease remains unknown, but it is believed to be influenced by a combination of genetic, environmental, and immune factors. These factors can also be considered risk factors for developing the condition.
Key Risk Factors
- Genetics: There is a strong genetic component to Crohn’s disease. Individuals with a family history of the condition are at a higher risk of developing it.
- Autoimmune Reaction: In Crohn’s disease, it’s believed that the immune system mistakenly identifies harmless gut bacteria or food particles as threats and launches an abnormal inflammatory response. This chronic inflammation leads to damage in the digestive tract.
- Environmental Factors: Certain environmental factors may trigger or exacerbate Crohn’s disease in genetically susceptible individuals. These factors may include diet, smoking, infections, or exposure to certain pollutants.
- Gut Microbiome: The composition of the gut microbiome, which is the community of microorganisms living in the digestive tract, has been implicated in Crohn’s disease. Changes in the balance of gut bacteria may influence the immune response and contribute to the development of inflammation.
Crohn’s disease is likely multifactorial, meaning that a combination of genetic predisposition and environmental triggers play a role in its onset. Ongoing research aims to gain a deeper understanding of the complex mechanisms behind this disease.
Diagnosis
The diagnosis of Crohn's disease typically involves a combination of several exams. Some common steps and methods used in the diagnostic process may include the following:
- Medical history and physical exam: : A healthcare provider will assess your symptoms, family history, and other relevant factors.
- Blood tests: To check for signs of inflammation, such as elevated C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR).
- Stool tests: To evaluate for infection, inflammation, or bleeding in the digestive tract.
- Imaging studies: To visualize the gastrointestinal tract and identify areas of inflammation or complications:
- Endoscopy: Colonoscopy or upper endoscopy to directly examine the affected areas and take biopsies.
- Small bowel imaging: CT enterography or magnetic resonance enterography (MRE) to visualize the small intestine.
- Biopsy: Tissue samples taken during endoscopy for microscopic examination to confirm inflammation and rule out other conditions.
It’s important to keep in mind that a thorough evaluation by a healthcare professional, including a gastroenterologist, is crucial to obtain an accurate diagnosis. Early diagnosis is key to initiating appropriate treatment and managing this disease effectively.
Treatment
The treatment of Crohn's disease aims to control symptoms, reduce inflammation, prevent complications, and improve the quality of life. The treatment plans can vary depending on the severity of your symptoms, the location and extent of inflammation, and individual factors.
Medications
- Aminosalicylates: Medications like mesalamine can help reduce inflammation in the gut.
- Corticosteroids: Short-term use of corticosteroids (e.g., prednisone) can quickly control inflammation during flare-ups. However, long-term use is generally avoided due to potential side effects.
- Immunosuppressants: Medications like azathioprine, mercaptopurine, or methotrexate can suppress the immune system and reduce inflammation.
- Biologic therapies: Medications like infliximab and adalimumab target specific molecules in the immune system to control inflammation. They are often used in moderate-to-severe cases or when other treatments are ineffective.
Nutritional Therapy
Exclusive enteral nutrition (EEN) involves consuming a liquid formula or special diet to provide all necessary nutrients while resting the digestive tract. It may be used in children or as an alternative to medications in specific cases.
Surgery
In some cases, surgery may be necessary to remove damaged or diseased portions of the intestine, address complications like strictures or fistulas, or manage severe symptoms that do not respond to other treatments.
Lifestyle Modifications
Adopting a healthy lifestyle can help manage symptoms and promote overall well-being. This includes maintaining a balanced diet, staying hydrated, managing stress levels, getting regular exercise, and avoiding tobacco use.
Symptom Management
Medications such as antidiarrheals, anti-gas, and pain relievers may be used to alleviate specific symptoms and improve quality of life.
Prevention
While there is no definitive way to prevent Crohn's disease, certain lifestyle choices may help reduce the risk or manage symptoms.
- Avoid tobacco: Smoking is a significant risk factor for Crohn's disease. Quitting smoking or avoiding tobacco use altogether can reduce your risk and improve treatment outcomes.
- Maintain a healthy diet: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support overall well-being and potentially reduce the risk of complications.
- Manage stress:Chronic stress has been linked to inflammatory bowel diseases. Effective stress management techniques, such as exercise, meditation, or counseling, can be beneficial.
- Breastfeeding: Some studies suggest that breastfeeding may have a protective effect against Crohn's disease in genetically predisposed children. Exclusive breastfeeding for the first few months can be considered.
Although these lifestyle choices can improve overall well-being and possibly lower the risk of Crohn's disease, they cannot guarantee prevention. If you are concerned about your risk of developing Crohn's disease or wish to manage your symptoms effectively, it’s recommended to speak with a healthcare professional. They can offer personalized advice and guidance tailored to your specific circumstances.
Related Topics
What is Inflammatory Bowel Disease?
Inflammatory Bowel Disease, or IBD, is a chronic condition caused by inflammation of the digestive system. IBD usually manifests in one of three different ways
Read moreLiving with a Chronic Illness
Living with a chronic disease can be challenging. The paths you take are often unique; every disease presents its own challenges, and every individual has their own experiences and barriers that they must overcome. Today I plan to share some of my own experiences in the hope that I can offer some helpful advice to those that may need it.
Read more