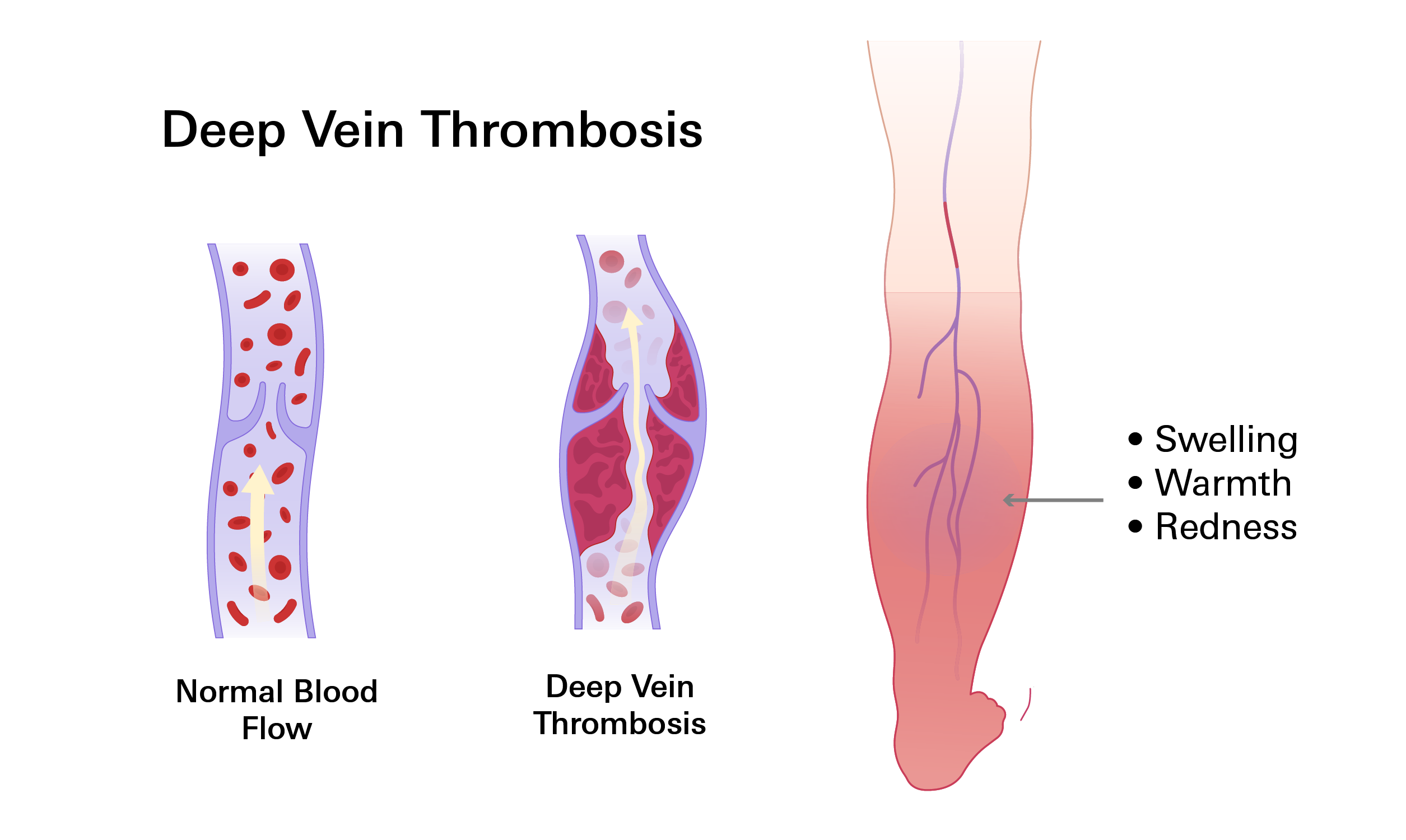
- Deep vein thrombosis (DVT) is the formation of a blood clot in a deep vein, typically in the legs.
- Symptoms include swelling, pain, redness, and warmth in the affected leg.
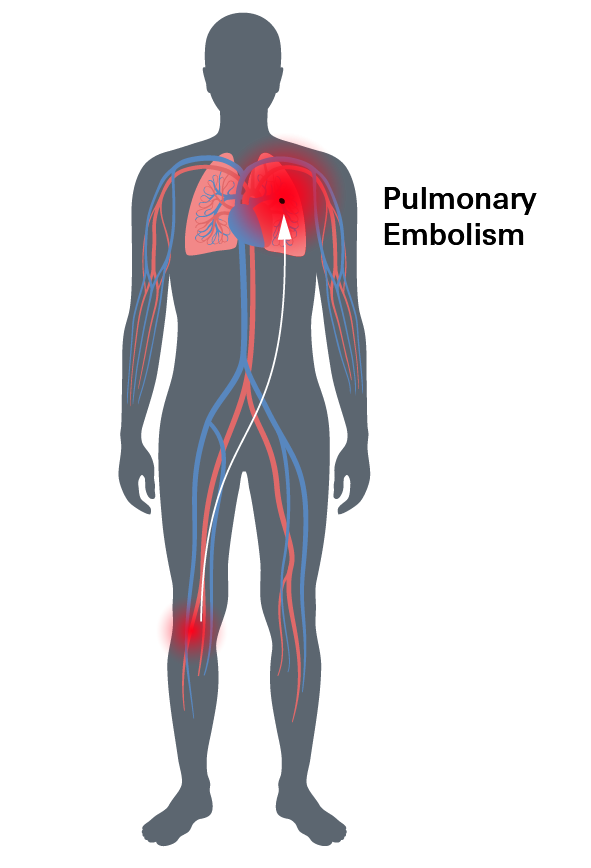
- The primary concern is that a clot can break loose and cause a pulmonary embolism (PE), a potentially life-threatening condition where the clot blocks arteries in the lungs.
- Risk factors include prolonged sitting, surgery, obesity, smoking, and certain medical conditions.
- Treatment typically involves blood thinners (anticoagulants) to prevent the clot from growing or breaking off.
- Prevention includes exercise, staying hydrated, avoiding smoking, and wearing compression stockings if at risk.
Overview
Deep vein thrombosis (DVT) is a serious condition where blood clots, known as thrombosis, form in the deep veins of the body, typically in the legs.
Imagine your veins as highways for blood to travel through your body. Sometimes, these highways can get clogged, similar to roads being blocked by a fallen tree. In DVT, these blockages occur inside the deep veins. This clotting can be painful and cause swelling in the affected area, making movement difficult and uncomfortable.
The danger with DVT is that if a clot breaks loose, it can travel through the bloodstream and become lodged in the lungs, a condition known as a pulmonary embolism (PE), which can be life-threatening.
Certain factors, such as prolonged sitting, extended bed rest, or specific medical conditions, can increase the risk of developing DVT.
DVT vs. PE
The most serious risk associated with DVT is a pulmonary embolism (PE). This occurs when a piece of the clot breaks loose and travels to your lungs, blocking blood flow. A PE can be life-threatening.
While DVT typically causes pain, swelling, and redness in the affected limb, PE can present with symptoms like sudden shortness of breath, chest pain, and coughing up blood. Both DVT and PE are serious medical conditions that require immediate treatment.
Prevalence
Deep vein thrombosis (DVT) is a surprisingly common condition. In the United States alone, an estimated 300,000 to 600,000 people are affected each year. Globally, the numbers are even more staggering, with millions of cases reported annually.
Several factors contribute to the widespread prevalence of DVT. Modern, sedentary lifestyles, rising obesity rates, and increasing average age populations all play a significant role. Additionally, genetic predispositions can increase an individual's risk.
Symptoms
Deep vein thrombosis (DVT) often presents with noticeable symptoms, but it's important to remember that not everyone experiences them. Common signs and symptoms include:
- Swelling: One leg, or occasionally both, may become swollen and feel heavy or tender.
- Pain or tenderness: You might experience cramping or soreness, often worsened by standing or walking.
- Warmth: The affected leg may feel warmer to the touch compared to the other leg.
- Redness: The skin over the clot may appear red or discolored.
- Visible veins: In some cases, veins near the skin's surface may become more prominent.
- Leg fatigue: You might feel unusual tiredness or heaviness in your leg.
- Skin discoloration: The skin may take on a bluish or reddish hue due to reduced blood flow.
If you experience any of these signs or symptoms, especially if they appear suddenly or worsen over time, seek medical attention immediately. DVT can lead to serious complications if left untreated.
Complications
DVT can lead to serious complications if left untreated or if the blood clot dislodges.
Pulmonary Embolism (PE)
The most dangerous complication of DVT is a pulmonary embolism (PE). This occurs when a piece of the blood clot breaks off and travels to the lungs, blocking blood flow. PE can cause severe symptoms such as shortness of breath, chest pain, and coughing up blood. In severe cases, it can be life-threatening.
Post-Thrombotic Syndrome
Another potential complication is post-thrombotic syndrome. This condition occurs when the DVT damages the veins, leading to ongoing problems such as leg pain, swelling, and skin changes.
Recurrent DVT
Individuals who have experienced one DVT are at an increased risk of developing another blood clot in the future.
It's crucial to be aware of these potential complications and to seek medical attention promptly if you suspect you may have DVT. Early diagnosis and treatment can significantly reduce the risk of complications.
Causes
Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, usually in your leg. This happens due to a combination of factors:
- Injury to the blood vessel wall: Damage to the inner lining of a vein can trigger clot formation.
- Changes in blood flow: Reduced blood flow, often caused by inactivity, can contribute to clot development.
- Alterations in blood composition: Changes in blood clotting factors can increase the risk of clot formation.
Risk Factors
Several factors can increase your risk of developing DVT:
- Sedentary lifestyle: Prolonged periods of sitting or immobility, such as long flights or bed rest, can slow blood flow and increase the risk of clots.
- Surgery and hospitalization: Major surgeries, especially those involving the legs or abdomen, can disrupt blood flow and increase the risk of DVT.
- Obesity: Excess weight can put pressure on your veins, hindering blood flow and raising the risk of clots.
- Smoking: Smoking damages blood vessels and increases the risk of blood clots.
- Family history: A family history of DVT or blood clotting disorders can increase your genetic predisposition.
- Hormones: Hormonal contraceptives and hormone replacement therapy can elevate the risk of blood clots.
- Pregnancy: Hormonal changes, increased pressure on pelvic veins, and decreased mobility during pregnancy can contribute to DVT.
- Medical conditions: Certain health conditions, including cancer, heart disease, inflammatory bowel disease, and autoimmune disorders, can increase the risk.
- Age: The risk of DVT increases with age due to changes in blood vessels and decreased activity levels.
Diagnosis
Diagnosing deep vein thrombosis (DVT) typically involves several diagnostic methods:
- Duplex Venous Ultrasound: This is the primary and preferred method or diagnosing DVT. It's a non-invasive test that uses sound waves to examine blood flow and identify blood clots in your veins. A healthcare professional applies pressure to the affected area while scanning it. If a blood clot is present, the vein will not compress properly.
- Venography: While less common due to its invasive nature, venography can be used in certain cases. This procedure involves injecting a contrast dye into your veins, allowing for clear visualization of blood flow and any blockages.
- Computed Tomography (CT) Scan: CT scans use X-rays to create detailed images of your body. They are helpful for detecting DVT in areas like your abdomen, pelvis, or brain, and for identifying pulmonary embolisms (blood clots in the lungs).
- Magnetic Resonance Imaging (MRI) or Magnetic Resonance Venography (MRV): These imaging techniques provide detailed images of your veins and surrounding tissues. They are often used when additional information is needed beyond what a duplex ultrasound or CT scan can provide.
In cases where a genetic or acquired clotting disorder is suspected, additional blood tests may be necessary. These tests are particularly important if you have a history of unexplained blood clots, blood clots in unusual locations, or a family history of blood clotting disorders.
Treatment
Treatment for DVT typically involves two primary phases: initial treatment and long-term management. The specific approach will depend on the severity of your DVT, your overall health, and other factors.
Initial Treatment (Hospital Setting)
The initial treatment typically begins in a hospital, especially for severe cases or those with underlying medical conditions. Doctors will likely administer Heparin, a medication that prevents blood clots from growing larger. Depending on the severity, medications to dissolve clots (Thrombolytics) may be used.
- Goal: To stabilize the condition and prevent the clot from growing or breaking off.
- Common treatments:
- Anticoagulants like heparin to prevent clot growth.
- Thrombolytic therapy (clot-busting drugs) in severe cases.
- Pain management.
- Compression stockings to reduce swelling.
Long-Term Management (Outpatient Care)
After your condition stabilizes, you might transition to outpatient care with regular doctor visits. Oral medications like Warfarin or Direct Oral Anticoagulants (DOACs) would likely be prescribed to continue blood clot prevention. You might also be advised to wear compression stockings to improve blood flow and reduce swelling.
- Goal: To prevent recurrent DVT and manage any ongoing symptoms.
- Common treatments:
- Continued use of anticoagulants, often transitioning from heparin to oral medications like warfarin or DOACs.
- Compression stockings.
- Lifestyle modifications, including exercise and weight management.
- Regular follow-up appointments with your healthcare provider.
Anticoagulants (Blood Thinners)
- Heparin: This is often the first medication given for DVT. It can be administered through an IV or as a subcutaneous injection. Side effects may include bleeding, heparin-induced thrombocytopenia (a rare but serious complication), and localized irritation at the injection site.
- Warfarin (Coumadin):This medication is typically started alongside heparin and taken orally. It takes at least 36 hours to start working and 4 to 5 days to reach its maximum effectiveness. Side effects may include bleeding, easy bruising, hair loss, and interactions with certain foods and medications.
- Direct-Acting Oral Anticoagulants (DOACs): Newer medications like rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa) are effective alternatives to warfarin and often require less monitoring.
- Rivaroxaban (Xarelto): Taken orally, generally once a day. Side effects may include bleeding, gastrointestinal discomfort, and liver enzyme abnormalities.
- Apixaban (Eliquis): Taken orally, generally twice a day. Common side effects include bleeding, nausea, and bruising.
- Dabigatran (Pradaxa): Another oral anticoagulant that inhibits thrombin. Side effects may include bleeding, gastrointestinal upset, and kidney dysfunction.
All anticoagulants carry a risk of bleeding, so they are carefully monitored and adjusted as needed.
Thrombolytic Therapy
Thrombolytic medications, often known as “clot busters,” work by dissolving the blood clot. These drugs have a higher risk of causing bleeding compared to anticoagulants and are typically reserved for severe cases of DVT.
Compressions
Wearing compression stockings or wraps can help reduce swelling and improve blood flow in the affected limb. Side effects are generally mild and may include skin irritation or discomfort.
Inferior Vena Cava (IVC) Filter
This surgical procedure involves inserting a device called a vena cava filter into the inferior vena cava to trap blood clots and prevent them from traveling to the lungs. This is usually considered when anticoagulants are not suitable or if there is a high risk of pulmonary embolism.
Lifestyle Changes
Adopting healthy lifestyle habits, such as regular exercise, maintaining a healthy weight, and avoiding prolonged periods of immobility, can help prevent DVT and manage your condition.
Prevention
Preventing DVT involves a combination of lifestyle modifications and medical interventions, especially for those at high risk.
Lifestyle Modifications
- Regular Physical Activity: Engaging in regular exercise, even light activity like walking or stretching, helps maintain good blood circulation and reduces the risk of blood clots.
- Hydration: Staying well-hydrated helps keep your blood flowing smoothly.
- Healthy Lifestyle Choices: Avoiding excessive alcohol consumption and smoking can contribute to overall vascular health.
Medical Interventions
For individuals at higher risk of DVT, such as those with a history of DVT, undergoing surgery, or having certain medical conditions, additional preventive measures may be recommended:
- Compression Stockings These can help improve blood flow in the legs and reduce the risk of clot formation.
- Anticoagulants: Blood thinners may be prescribed to prevent blood clots from forming.
- Regular Medical Assessments: Monitoring for signs of DVT is crucial, especially for high-risk individuals.
By incorporating these preventive measures into your lifestyle, you can significantly reduce your risk of developing DVT.
Related Topics
Anticoagulants Explained: When and Why They Are Used
Anticoagulants are used to prevent these dangerous types of clots. These medications are prescribed for individuals at high risk of forming abnormal blood clots due to conditions like atrial fibrillation (an irregular heartbeat), deep vein thrombosis (DVT), or those who have already suffered a heart attack or stroke.
Read moreBlood Thinners Don’t Really “Thin” Blood
Blood thinners work by interfering with the normal clotting process in your body. They do not actually "thin" your blood, but rather slow down the formation of clots. There are different types of blood thinners, but they all have a similar goal: to prevent clots from getting too big or forming in the wrong places.
Read more