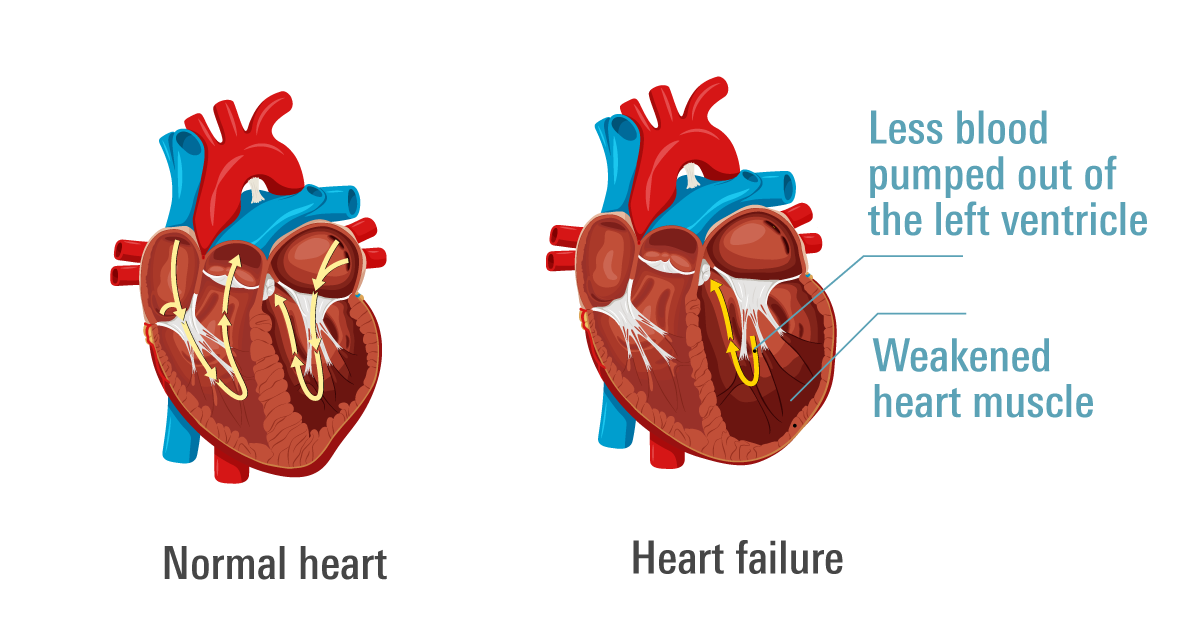
- Heart failure is a condition where the heart is unable to pump blood effectively to the body's cells.
- Common symptoms include shortness of breath, fatigue, swelling in the legs and ankles, rapid heartbeat.
- Risk factors include age, family history, lifestyle factors (smoking, poor diet, lack of exercise), and certain medical conditions.
- Treatment aims to manage symptoms, improve quality of life, and prevent the condition from worsening. Treament options include medications, lifestyle changes (healthy diet, regular exercise), and cardiac rehabilitation.
Overview
Heart failure (congestive heart failure) does not mean your heart has ‘failed’ or stopped working. It is a condition in which your heart is not pumping blood as well as it should. The condition can be acute or chronic. This condition can be chronic (long-term) or acute, leading to symptoms such as coughing, shortness of breath, and exhaustion. These symptoms can make everyday activities like carrying groceries, walking, and climbing stairs extremely challenging.
Acute heart failure is a medical emergency and needs immediate attention. Chronic heart failure develops over time and causes symptoms such as coughing, shortness of breath, and exhaustion. Your daily tasks like carrying groceries, walking, and climbing stairs can become exceedingly challenging.
Some common causes of heart failure are coronary artery disease, high blood pressure, diabetes, and obesity. Treatment typically involves a combination of lifestyle changes, and medications.
Prevalence
Heart failure is a significant health concern in the United States, affecting over 6.5 million Americans over the age of 20. Each year, approximately 960,000 new cases are diagnosed. According to the American Heart Association, the prevalence of heart failure is expected to rise substantially by 2030. This increase is attributed to factors such as the aging population and the prevalence of conditions that contribute to heart failure, including coronary artery disease (CAD), high blood pressure, diabetes, and obesity. Managing these underlying conditions is crucial in preventing and controlling heart failure.
Symptoms
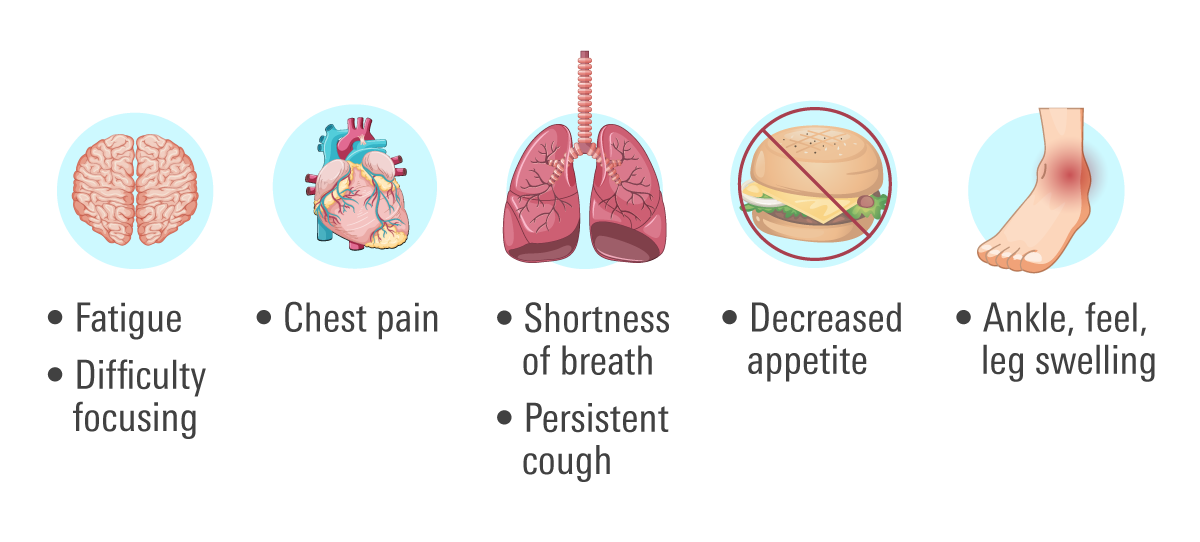
- Shortness of breath (SOB), which may occur while exercising or during rest
- Difficulty breathing
- Nausea
- Exhaustion or weakness
- Swelling that may occur in your ankles, legs, and/or feet
- A pulse or heartbeat that may be fast or inconsistent
- Decreased stamina for exercise
- A cough that may be persistent or wheezing with blood-tinged mucus that is either white or pink
- Abdominal swelling or bloating
- Increased weight
- Decreased appetite
- Having trouble focusing or being less alert
Stages
There are two classifications for stages of heart failure:
NYHA Functional Classification
The New York Heart Association Functional Classification is older, simpler and more widely used in clinical settings due to its simplicity. It consists of four stages based on patient’s self-reported symptoms.
It’s also used as a base for various drug studies, and highly significant to choices regarding drug therapy.
| NYHA Functional Classification | |
| Class I | No limitations of physical activity. |
| Class II | Slight limitation of physical activity. Comfortable at rest. Regular physical activity causes symptoms. |
| Class III | Marked limitation of physical activity. Comfortable at rest. Less than regular physical activity causes symptoms. |
| Class IV | Symptoms occur even at rest, discomfort with any physical activity. |
ACC/AHA Stages
The American Heart Association and American College of Cardiology defined the four stages of heart failure in 2001.
It provides more a comprehensive picture of patient’s condition since it considers patient’s functional impairment as well as their symptoms.
| ACC/AHA Stages | |
| Stages | Treatment |
| Stage A High risk of heart failurewithout heart disease or HF symptoms |
|
| Stage B
Structural heart disease but no signs or symptoms of heart failure. |
|
| Stage C
Structural heart disease with symptoms of heart failure. |
|
| Stage D
Advanced heart failure requiring specialized interventions. |
|
Risk Factors
Heart failure can affect both men and women equally, although men are more likely to develop it earlier in life. Several factors can increase the likelihood of developing heart failure, especially when multiple factors are present.
Genetics
A family history of heart failure can significantly increase your risk. Certain genetic mutations can cause your heart tissue to become weaker or less flexible, making it more susceptible to heart failure.
Aging
As you age, your heart may become stiffer and weaker. Individuals over the age of 65 are at a higher risk of heart failure. Additionally, older adults are more prone to medical conditions that can lead to heart failure.
Lifestyle
Unhealthy lifestyle choices are major risk factors for heart failure. These include poor eating habits, smoking, using cocaine or other illicit substances, excessive alcohol consumption, and lack of physical activity.
African Americans
African Americans are more likely than individuals of other races to develop heart failure. They also tend to experience more severe cases and at a younger age.
Diagnosis
Cardiologists typically use a combination of medical history, physical examination and diagnostic tests in order to diagnose heart failure.Your doctor will ask you about your symptoms, look for conditions like diabetes, coronary artery disease, or high blood pressure that might be possible causes of heart failure.During physical examination your doctor can check your heart for murmurs that can indicate heart failure as well as your lungs for indications of fluid accumulation (lung congestion).
Additionally, your specialist could recommend a few of the following tests:
- Blood test
To check for abnormalities that may harm your heart.
- Electrocardiogram (ECG)
ECG captures electrical cardiac impulses and displays the frequency and duration of your heartbeats.
- Echocardiography (ECHO)
ECHO uses sound waves to create visuals of your heart. This analysis is performed when heart failure is suspected and it's used to reveal the size, shape, and blood flow through your heart and heart valves.
It shows how much blood is pushed out of the heart through the left ventricle—the primary pumping chamber—with each contraction.
A normal ejction fraction is 53% to 70%. An ejctions fraction less than 40% indicates systolic dysfunction or heart figure with reduced ejection fraction (HFrEF), meaning your heart doesn't pump blood to your body as efficiently as it should.
- Chest X-ray
Images show health of your heart and lungs.
- Stress test
A cardiac test that evulates how well the heart works during exercise.
You wear a ECG monitor while walking on a treadmill.
- CT scan
A CT scan is used to produce precise images of your heart and its blood vessels.
- MRI
A dye (contrast) may be used to conduct a cardiac MRI.
It's crucial to let your doctor know if you have any renal issues since contrast can sometimes result in rare but significant problems that may arise in individuals with kidney disease.
- Coronary angiogram
This procedure involves inserting a thin, flexible tube (catheter) into a blood artery, typically in the groin, and directing it to your heart arteries. A dye (contrast) is administered through the catheter to assist your specialist in identifying obstructions by making the arteries appear more clearly on an X-ray.
Treatment
Heart failure treatment aims to alleviate symptoms, improve quality of life, and prevent the condition from worsening, thereby reducing the risk of death and hospitalization.
Medications
- ACE inhibitors (angiotensin-converting enzyme inhibitors): Help relax blood vessels and reduce the workload on the heart.
- Aldosterone receptor antagonists (ARAs): Block the effects of aldosterone, a hormone that can cause salt and fluid retention.
- ARBs (angiotensin II receptor blockers): Similar to ACE inhibitors, they help relax blood vessels.
- ARNIs (angiotensin receptor-neprilysin inhibitors): Combine the effects of ARBs and neprilysin inhibitors to enhance heart function.
- Beta-blockers: Reduce heart rate and blood pressure, decreasing the heart’s workload.
- Digoxin: Helps the heart pump more effectively and controls heart rate.
- Calcium channel blockers: Relax blood vessels and reduce heart rate.
- Diuretics, including loop diuretics: Help remove excess fluid from the body, reducing the strain on the heart.
- Ivabradine (brand: Corlanor): Lowers heart rate and improves heart function.
- Hydralazine and nitrates (generic: BiDil): Relax blood vessels and improve blood flow.
Lifestyle Changes and Cardiac Rehabilitation
In addition to medications, lifestyle changes are crucial in managing heart failure. Your cardiologist may recommend a cardiac rehabilitation program, which includes:
- Personalized Exercise Plans: Tailored exercises to improve cardiovascular health.
- Education and Counseling: Information on how to reduce cardiac risk factors, such as quitting smoking and adopting a heart-healthy diet.
- Support: Guidance on managing stress and making sustainable lifestyle changes.
By combining these treatments and lifestyle modifications, individuals with heart failure can significantly improve their quality of life and manage their condition more effectively.
Prevention
The actions listed below can help reduce your chance of getting heart failure. Keep in mind that your chances of preventing or delaying the disease are higher the earlier you begin.
- Choosing a heart-healthy approach. Your heart's health may be maintained by consuming heart-healthy meals (eating fruits and vegetables (4 servings a day)), working toward a healthy weight, engaging in regular physical exercise (≥ 5 days a week), stopping smoking, and managing stress.
- Do not take illicit substances (including cocaine and amphetamine abuse), and limit or avoid drinking alcohol (limit to 1 drink a day).
- Limit the amount of caffeine consumption (≤ 4 cups a day).
- Manage your risk of heart failure by working with your doctor to control diseases including diabetes, high blood pressure or hypertension, and obesity.
3 Myths Debunked on Heart Disease
Many problems involving the heart are associated with a process known as atherosclerosis. According to the American Heart Association, atherosclerosis “is a condition that develops when a substance called plaque builds up in the walls of the arteries. This buildup narrows the arteries, making it harder for blood to flow through. If a blood clot forms, it can block the blood flow. This can cause a heart attack or stroke.”
Read moreJardiance for Type 2 Diabetes and Congestive Heart Failure
Jardiance is the brand name for the medication empagliflozin. It is primarily used to treat type 2 diabetes mellitus, a condition in which the body is unable to properly regulate blood sugar levels. Jardiance belongs to a class of medications called sodium-glucose co-transporter 2 (SGLT2) inhibitors.
Read moreInpefa, known as Sotagliflozin, is a prescription medication classified under the drug category of sodium-glucose co-transporter 1 and 2 inhibitors (SGLT1/SGLT2 inhibitors). It helps manage type 2 diabetes by regulating blood glucose levels.
Read more