- Hemorrhoids are swollen and inflamed blood vessels in the lower rectum and anus. They can cause discomfort, bleeding, and itching.
- Common causes include straining during bowel movements, pregnancy, and a low-fiber diet.
- Risk factors include age, obesity, and a sedentary lifestyle.
- Over-the-counter medications like creams and suppositories can help relieve symptoms. In more severe cases, procedures like rubber band ligation or surgery may be necessary.
Overview
Hemorrhoids occur when the blood vessels in the lower rectum and anus become swollen and irritated.
The rectum and anus are the final parts of the digestive system. Inside their walls are veins, called hemorrhoidal veins, that provide support and cushioning. These veins, along with surrounding muscles, help control bowel movements by keeping the anus closed until it's time to pass stool.
Normally, these veins expand and contract easily to allow stool to pass. However, excessive pressure on these veins can cause them to swell and inflame, leading to hemorrhoids. This pressure can result from straining during bowel movements, prolonged sitting, or chronic constipation. When this happens, blood pools in the hemorrhoidal veins, causing them to bulge.
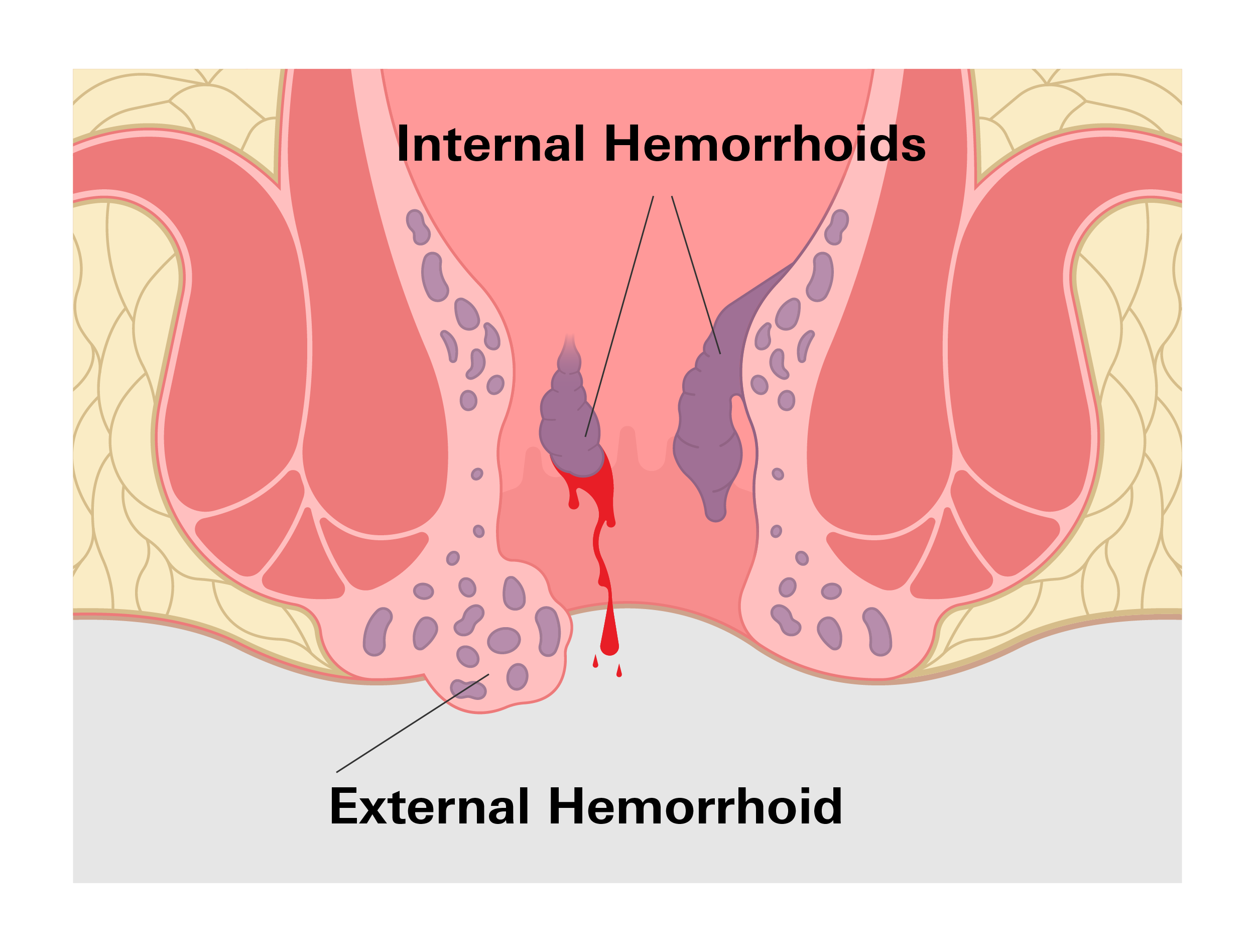
There are 2 types of hemorrhoids: internal and external.
- Internal Hemorrhoids: Located inside the rectum, they often cause painless bleeding, especially during bowel movements.
- External Hemorrhoids: Located under the skin around the anus, they can cause discomfort, itching, swelling, and pain, especially if a blood clot forms (thrombosed hemorrhoid).
The cushion of veins in the rectum and anus normally helps with continence by providing support and helping the muscles in this area to close off the anus when we are not having a bowel movement. However, when hemorrhoids form, this process can be disrupted, leading to discomfort, pain, or other symptoms.
Remember that hemorrhoids are a common condition, and although they can be uncomfortable, they are usually not dangerous and can often be managed with proper care.
Prevalence
Hemorrhoids are a common condition affecting millions of Americans. It is estimated that about 1 in 20 Americans will experience hemorrhoids at some point in their life, with the prevalence increasing as people age. Nearly half of all adults over 50 are likely to experience them.
Hemorrhoids can affect both men and women, though certain groups, such as pregnant women, are at higher risk. During pregnancy, the increased pressure on the pelvic veins and hormonal changes make hemorrhoids more likely to develop, especially in the third trimester.
Additionally, those with chronic constipation, obesity, or those who frequently engage in heavy lifting or prolonged sitting may be more susceptible to hemorrhoids.
Symptoms
The signs and symptoms of hemorrhoids can vary depending on their location and severity. While they are often uncomfortable, symptoms can vary widely, from mild irritation to more intense pain or bleeding.
- Rectal Bleeding: Painless, bright red blood during or after bowel movements, often a sign of internal hemorrhoids. It is important to note that while rectal bleeding is a common sign of hemorrhoids, any bleeding from the rectum should be evaluated by a doctor to rule out more serious conditions.
- Itching and Irritation: Persistent itching around the anus is a common symptom of external hemorrhoids. This occurs because the swollen veins irritate the sensitive skin in this area. The presence of mucus or stool leakage due to incomplete closure of the anus can also cause itching, further worsening the irritation.
- Pain or Discomfort: More common with external hemorrhoids, especially when sitting or during bowel movements. This discomfort can range from mild tenderness to more severe, sharp pain, particularly if the hemorrhoid becomes thrombosed (clotted). Internal hemorrhoids generally don’t cause pain unless they prolapse, or fall outside the anus.
- Swelling or Lumps: Visible or palpable lumps near the anus, often associated with external hemorrhoids. These lumps are swollen veins filled with blood and can be tender to the touch. Oftentimes, a thrombosed hemorrhoid will appear as a bluish or purplish lump due to the blood clot inside it, causing significant pain and inflammation.
- Prolapse: Internal hemorrhoids can sometimes prolapse, meaning they push through the anus and become visible or palpable outside the body. Prolapsed hemorrhoids may retract on their own, or they may need to be gently pushed back inside. If left untreated, a prolapsed hemorrhoid can cause ongoing discomfort and may lead to more serious complications, such as strangulation, where the blood supply to the hemorrhoid is cut off.
- Mucus Discharge: A slimy discharge, especially after bowel movements, can irritate the skin. Mucus leakage is more likely to occur when internal hemorrhoids prolapse.
- Incomplete Bowel Movement: A feeling of incomplete evacuation due to hemorrhoids blocking the anal opening. This can lead to straining, which may worsen the hemorrhoids.
Keep in mind that these symptoms can vary in intensity and may come and go depending on the severity of the hemorrhoids. While mild cases might cause occasional discomfort or irritation, more severe hemorrhoids can lead to persistent pain, bleeding, or complications that require medical treatment. Recognizing these signs early on can help prevent worsening symptoms and guide appropriate treatment steps.
Causes
Hemorrhoids are caused by too much pressure on the veins in the lower rectum and anus. These veins are normally flexible and allow blood to flow easily. But when the pressure increases, the veins can swell, stretch, and sometimes even bulge out, leading to hemorrhoids.
There are several common reasons why this pressure builds up. One major cause is straining during bowel movements, which often may occur when you are constipated. When the stool is hard or difficult to pass, you may tend to push harder, and this extra strain puts pressure on the veins. On the other hand, having diarrhea frequently can also irritate these veins because of the constant bowel movements.
Sitting for long periods, especially on the toilet, can also contribute to hemorrhoids. When you sit for too long, it can slow blood flow in the veins, causing them to swell. Those with jobs that require long periods of sitting, including office workers or truck drivers, are more likely to experience hemorrhoids.
Pregnancy is another common cause. As the baby grows, it puts pressure on the mother’s pelvic area, including the rectal veins, which can cause hemorrhoids to develop. Hormonal changes during pregnancy can also make the veins more prone to swelling.
Other factors include obesity, which puts extra weight and pressure on the lower body, and heavy lifting, which can strain the veins in the rectum. A diet low in fiber can also play a role because it leads to constipation and harder stool, which increases the likelihood of straining.
All of these causes share one thing in common: they increase the pressure in the veins around the rectum and anus, making hemorrhoids more likely to form.
Risk Factors
While anyone can develop hemorrhoids, certain factors increase the risk:
- Age: As we age, the tissues supporting the rectal veins weaken and stretch, making hemorrhoids more common in older adults. This is why hemorrhoids are more common in adults over the age of 50.
- Constipation and Diarrhea: Both conditions can strain the rectal veins. Constipation can lead to straining during bowel movements, which increases pressure on these veins. Diarrhea, on the other hand, causes irritation and frequent bowel movements, which can also contribute to hemorrhoid formation.
- Pregnancy: Hormonal changes and increased pressure on pelvic veins during pregnancy can lead to hemorrhoids. Hemorrhoids are especially common in the third trimester and right after childbirth.
- Obesity: Excess weight can put additional pressure on the veins.
- Sedentary Lifestyle: Prolonged sitting can slow blood flow in the rectal veins.
- Low-Fiber Diet: A low-fiber diet can lead to constipation and straining. Fiber helps soften stool and helps with regular bowel movements, reducing the risk of hemorrhoids.
- Heavy Lifting: Straining during heavy lifting can increase pressure on the rectal veins.
- Genetics: A family history of hemorrhoids may increase your risk.
Remember that these risk factors do not necessarily guarantee that you will develop hemorrhoids, however, being aware of them can help you make lifestyle changes to lower your risk and manage symptoms early.
Diagnosis
If you visit your doctor with symptoms such as rectal bleeding, discomfort, or swelling, they will first ask about your symptoms, how long you've had them, and whether you've noticed any patterns, such as pain during bowel movements or itching around the anus. This helps them understand whether hemorrhoids are the likely cause or if another condition might be responsible for the symptoms.
The next step is generally a physical exam. For external hemorrhoids, the doctor can often diagnose the condition by simply looking at the area around the anus. External hemorrhoids are usually visible and may appear as swollen, discolored lumps.
For internal hemorrhoids, which are located inside the rectum and not visible from the outside, a digital rectal exam may be performed. During this exam, the doctor gently inserts a gloved, lubricated finger into the rectum to feel for any abnormalities, including swollen or tender veins.
In some cases, if the diagnosis is unclear or if there are concerns about other conditions, including polyps or colorectal cancer, your doctor may recommend additional diagnostic procedures. One common test is called an anoscopy, where a small, lighted tube is inserted into the anus to give the doctor a clearer view of the internal hemorrhoids. Another option is a sigmoidoscopy or colonoscopy, which examines a larger portion of the lower digestive tract. These tests are typically used if there is significant bleeding or if the doctor suspects other issues beyond hemorrhoids.
Accurate diagnosis is important not only for determining the best treatment for hemorrhoids but also for ruling out more serious conditions that can cause similar symptoms, such as colorectal cancer.
Treatment
Hemorrhoid treatments vary depending on the severity and location of the hemorrhoids, with options ranging from at-home care to medications and medical procedures.
Over-the-Counter Treatments
OTC treatments for hemorrhoids focus on relieving symptoms such as pain, swelling, and itching. These products contain active ingredients specifically designed to target inflammation, soothe irritation, or reduce swelling, making them effective for managing mild to moderate hemorrhoids.
These topical treatments are applied directly to the affected area and are among the most popular for external hemorrhoids, providing immediate relief and protection for irritated skin.
Common active ingredients include the following:
- Hydrocortisone: A mild corticosteroid that reduces inflammation, itching, and swelling, hydrocortisone creams are recommended for hemorrhoids as they directly address the root of inflammation.
- Phenylephrine: This vasoconstrictor, found in products such as Preparation H, works by narrowing swollen blood vessels, helping to reduce the size and discomfort of the hemorrhoid.
Hemorrhoid pads and wipes are convenient for managing symptoms throughout the day, especially for external hemorrhoids, as they are easy to use and portable.
Common active ingredients include the following:
- Witch hazel:Known for its astringent and anti-inflammatory properties, witch hazel helps reduce swelling and soothes the affected area.
- Aloe vera: Gentle and moisturizing, aloe vera helps hydrate and calm irritated skin, making it ideal for external hemorrhoids.
Examples of popular OTC products include:
- Preparation H ointment: This ointment provides symptom relief through phenylephrine, which reduces swelling, and mineral oil and petrolatum, which create a protective barrier.
- Preparation H suppositories: Designed for internal hemorrhoids, these suppositories target the area within the rectum, containing phenylephrine to reduce swelling and cocoa butter to soothe internal tissues
- Preparation H cooling gel: This gel provides a cooling effect for quick relief, with witch hazel and aloe vera to reduce swelling and calm external hemorrhoids.
- Preparation H max strength cream: For intense symptoms, this cream combines phenylephrine with pramoxine HCl, a numbing agent, to relieve pain and itching.
- Tucks medicated cooling pads: These pads offer on-the-go relief, containing witch hazel and aloe vera to reduce swelling and soothe irritated skin.
At-Home Treatments and Lifestyle Changes
In addition to OTC medications, several home remedies and lifestyle modifications can help alleviate hemorrhoid symptoms and prevent future occurrences.
- Sitz baths: Soaking the anal area in warm water for 10-15 minutes, several times a day, helps reduce inflammation and improve blood flow, relieving discomfort.
- Cold compresses: Applying a cold pack to the affected area can reduce swelling and numb pain, especially helpful after bowel movements.
- Fiber-rich diet: Increasing dietary fiber with fruits, vegetables, and whole grains softens stool, making bowel movements easier and reducing strain on hemorrhoidal veins. This helps prevent constipation, which is a common trigger for hemorrhoids.
Medical Procedures (for severe cases)
For persistent or severe hemorrhoids that do not respond to OTC or at-home treatments, medical procedures may be necessary. These interventions are typically performed by a healthcare professional and are effective for advanced hemorrhoids, particularly when pain, bleeding, or prolapse becomes a concern.
- Rubber band ligation: This procedure involves placing a rubber band around the base of an internal hemorrhoid, cutting off its blood supply, which causes it to shrink and fall off.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid, which causes the blood vessel to collapse and shrink over time. This is often used for smaller internal hemorrhoids.
- Infrared coagulation: Heat from infrared light is applied to the hemorrhoid, causing it to shrink. This procedure is most effective for smaller internal hemorrhoids.
- Hemorrhoidectomy: In severe cases, particularly when large hemorrhoids are present, surgical removal may be recommended. This procedure removes both internal and external hemorrhoids and is considered the most effective for chronic or large hemorrhoids.
- Hemorrhoidopexy (Stapled hemorrhoid surgery): Often used for prolapsed hemorrhoids, this procedure uses a stapling device to reposition the hemorrhoid and cut off its blood supply, which allows it to shrink and heal.
Complications
Although hemorrhoids are often manageable and not life-threatening, they can lead to complications if left untreated or if they worsen over time.
One of the most common complications is anemia, which can occur due to chronic blood loss from internal hemorrhoids. While the bleeding is usually minimal, it can lead to iron deficiency and fatigue if it continues over an extended period.
Another potential complication is a strangulated hemorrhoid, which happens when an internal hemorrhoid prolapses and becomes trapped outside the anus, cutting off its blood supply. This condition can cause severe pain and may lead to tissue death, requiring immediate medical intervention.
Thrombosis is another serious complication, particularly for external hemorrhoids. This occurs when a blood clot forms inside the hemorrhoid, causing it to become hard, swollen, and extremely painful. In some cases, the clot may need to be surgically removed to alleviate the discomfort.
Additionally, hemorrhoids that prolapse or remain untreated can lead to persistent irritation, skin tags, or infections in the area.
In rare cases, hemorrhoids can cause chronic discomfort that significantly impacts quality of life, making it essential to seek appropriate treatment to prevent these complications from developing.
Prevention
Preventing hemorrhoids largely revolves around maintaining healthy bowel habits and reducing strain on the rectal and anal veins.
One of the most effective ways to prevent hemorrhoids is by regular, soft bowel movements. This can be achieved through a diet high in fiber, which helps keep stool soft and easy to pass, minimizing the need for straining during bowel movements. Foods rich in fiber, such as fruits, vegetables, whole grains, and legumes, can significantly reduce the risk of constipation, a major factor in the development of hemorrhoids. Staying well-hydrated is also essential, as water helps to keep stool soft and prevents constipation.
In addition to dietary changes, regular physical activity can improve digestive health and help prevent constipation, further reducing pressure on the hemorrhoidal veins. It is also important to avoid sitting for prolonged periods, especially on the toilet. Sitting for too long can cause blood to pool in the veins of the rectum and anus, increasing the risk of hemorrhoids. When using the toilet, try not to strain or push too hard, as this creates unnecessary pressure on the veins.
Establishing a healthy bathroom routine can also help prevent hemorrhoids. Going to the bathroom as soon as you feel the urge to have a bowel movement can prevent straining caused by holding in stool.
By adopting these simple lifestyle changes, you can significantly reduce the likelihood of developing hemorrhoids and maintain overall digestive health.
Related Topics
What Can You Do About Hemorrhoids?
The development of hemorrhoids is linked to changes in blood flow and pressure within the veins of the lower rectum and anus.
Read moreTop OTC Medications for Hemorrhoid Relief
OTC treatments for hemorrhoids are designed to relieve symptoms such as pain, itching, and swelling. Many of these products contain active ingredients that target inflammation, provide soothing relief, or protect the affected area from further irritation.
Read more