- Hidradenitis suppurativa (HS) is a chronic skin condition causing painful bumps, nodules, and abscesses in skin folds.
- Symptoms includes painful lumps, pus-filled sores, tunnels under the skin, scarring.
- The exact causes are unknown, but it's thought to be linked to hair follicle inflammation, bacterial infection, and genetic factors..
- HS is more common in women, typically starts after puberty, and associated with obesity and smoking..
- Treatment includes medications (antibiotics, TNF-alpha inhibitors, hormonal treatments), surgical options, laser therapies, and lifestyle changes.
Overview
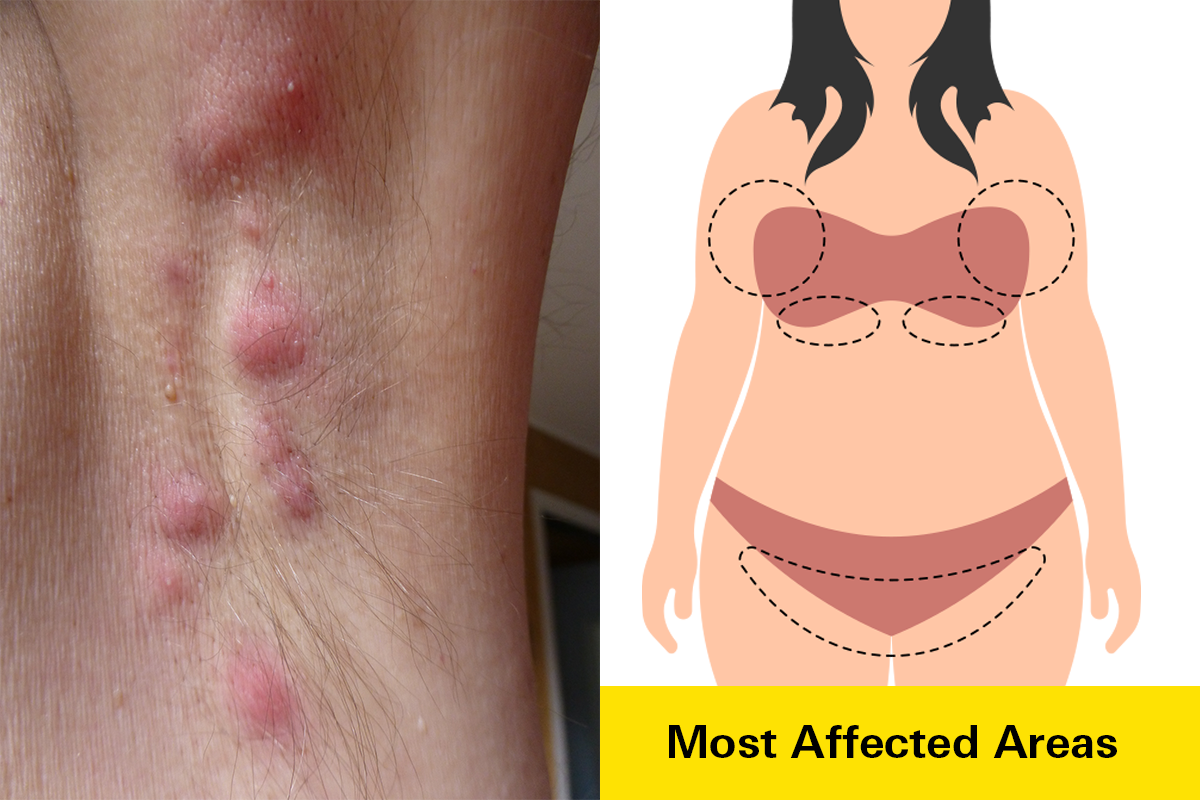
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic and often painful skin condition. It causes the formation of inflamed bumps, nodules, and abscesses (swollen collections of pus) deep within the skin. These typically occur in areas where skin rubs together, such as the armpits, groin, inner thighs, buttocks, and under the breasts.
Over time, these lesions can rupture, leading to the development of tunnels or tracts beneath the skin. HS can significantly impact a person's physical and emotional well-being due to its painful and recurrent nature.
While HS can develop at any age, it commonly begins after puberty, often in the late teens or early twenties. However, onset can occur later in life, sometimes even in the thirties or forties. The condition is more prevalent in women than men, and people of African descent are at a higher risk compared to other racial groups.
Left untreated, HS can worsen, resulting in the formation of multiple abscesses. When these rupture, they often leave behind scars and can lead to the development of subcutaneous tunnels known as sinus tracts. Early medical intervention, typically by a dermatologist, is crucial to manage symptoms, prevent complications, and improve quality of life.
Prevalence
Hidradenitis suppurativa (HS) is considered a relatively rare condition. While exact prevalence rates vary, it is estimated to affect approximately 1% of the population in the United States. It's important to note that these figures may underestimate the true prevalence due to underdiagnosis and underreporting.
Symptoms
Hidradenitis suppurativa (HS) is characterized by a range of symptoms that can vary in severity from person to person. Common signs and symptoms include:
- Painful bumps and nodules: These often develop in areas where skin rubs together, such as the armpits, groin, and buttocks. They can be red, swollen, and tender.
- Abscesses: Filled with pus, these painful lumps can form deep within the skin. When they rupture, they may release an unpleasant odor.
- Tunnels or tracts: These are abnormal passages that can develop beneath the skin, connecting abscesses.
- Scarring: As HS progresses, thick, rope-like scars may form on the affected areas.
- Skin changes: The skin in affected areas may become thickened, darkened, and inflamed.
- Pain and discomfort: HS can cause significant pain and discomfort, which can interfere with daily activities.
- Restricted mobility: In severe cases, the pain and swelling associated with HS can limit range of motion and daily activities.
It's important to note that HS symptoms can fluctuate in intensity and frequency. Some individuals may experience periods of remission when symptoms improve or disappear, followed by flare-ups.
Causes
The exact cause of hidradenitis suppurativa (HS) remains unknown, but it's believed to involve a ccombination of genetic, hormonal, and environmental factors. The condition typically begins with inflammation of hair follicles in areas where skin rubs together.
- Hair follicle inflammation: Inflammation of hair follicles is a central component of HS. This inflammation can be triggered by various factors, including friction, hormonal changes, and genetic predisposition.
- Follicular blockage: As inflammation progresses, hair follicles become blocked, trapping sweat, oil, and dead skin cells. This creates an environment for bacteria to thrive.
- Bacterial involvement: While not the primary cause, bacteria play a role in worsening HS. They contribute to the formation of painful abscesses and the release of pus.
Risk Factors
Several factors can increase a person's risk of developing HS or experiencing more severe symptoms.
- Genetics: A family history of HS is a significant risk factor, suggesting a genetic component to the condition.
- Hormonal factors: Hormonal changes, such as those occurring during puberty, menstruation, or pregnancy, can influence HS development or severity.
- Obesity: Excess weight is associated with a higher risk of HS, likely due to increased skin-to-skin friction and inflammation in skin folds.
- Smoking: Cigarette smoking is a well-established risk factor for HS and can worsen symptoms.
- Friction and sweating: Activities or conditions that cause excessive sweating or skin-to-skin friction can irritate affected areas and contribute to HS development.
It's important to note that having one or more of these risk factors does not guarantee the development of HS. Many people with these factors never develop the condition.
Diagnosis
Diagnosing hidradenitis suppurativa (HS) can be challenging as its symptoms often resemble other skin conditions, such as acne, boils, or infections. However, a healthcare professional, typically a dermatologist, can accurately diagnose HS based on a thorough examination and medical history.
Diagnostic Process
- Physical Examination: A dermatologist will carefully examine the affected areas of your skin. They will look for characteristic features of HS, such as painful bumps, nodules, abscesses, and tunnels.
- Medical History: Your doctor will ask about your symptoms, including when they started, their severity, and any factors that seem to worsen them. They may also inquire about your family history of skin conditions.
- Differential Diagnosis: To rule out other possible conditions, your doctor may consider factors like your age, overall health, and location of the skin lesions.
- Laboratory Tests: While there's no specific test for HS, your doctor might order blood tests or cultures to rule out other infections or underlying conditions.
Challenges in Diagnosis
HS can often be misdiagnosed due to its similarity to other skin conditions. This delay in diagnosis can lead to unnecessary treatments and prolonged discomfort. It's essential to seek the expertise of a dermatologist for an accurate diagnosis and appropriate treatment plan.
Treatment
Hidradenitis suppurativa (HS) is a complex condition that often requires a multi-faceted treatment approach. The best treatment plan will depend on the severity of your condition and your individual needs.
Medical Treatments
- Topical medications: These are applied directly to the skin to reduce inflammation and bacteria. Common options include clindamycin and resorcinol.
- Oral antibiotics: Antibiotics like doxycycline, minocycline, and erythromycin can help control bacterial infections and reduce inflammation.
- Hormonal therapies: Birth control pills, spironolactone, and anti-androgens can be beneficial for some women.
- Biologic agents: Medications like adalimumab (Humira) target specific immune system proteins to reduce inflammation.
- Steroid injections: Corticosteroid injections can help reduce swelling and pain in individual lesions.
- Other medications: Metformin, a drug typically used for diabetes, has shown promise in managing HS.
- Botox: Can decrease sweating, which may reduce flare-ups.
Surgical Treatments
- Incision and drainage: This procedure is used to drain abscesses and remove pus.
- Laser surgery: Can be used to reduce inflammation and improve symptoms. Medications are often prescribed to stabilize the condition before surgery for optimal results.
- Surgical excision: Removal of affected skin and underlying tissue may be necessary in severe cases.
- Laser hair removal: This therapy reduces hair on the skin, leading to fewer lumps and flare-ups.
Lifestyle Modifications
- Weight management: Maintaining a healthy weight can reduce friction and inflammation in skin folds.
- Smoking cessation: Smoking can worsen HS symptoms, so quitting is beneficial.
- Gentle skin care: Using mild cleansers and avoiding harsh scrubbing can help prevent irritation.
- Loose-fitting clothing: Wearing breathable fabrics can reduce friction and sweat buildup.
Prevention
While HS cannot be entirely prevented due to its complex nature, adopting healthy lifestyle habits and early intervention can help manage symptoms and reduce the risk of flare-ups.
- Maintain a healthy weight: This can help reduce friction and inflammation in skin folds.
- Quit smoking: Smoking is linked to more severe HS, so quitting can be beneficial.
- Practice good hygiene: Keeping the skin clean and dry can help prevent infections.
- Early treatment: Seeking medical attention at the first signs of HS can help prevent the condition from worsening.
- Avoid tight clothing: Wearing loose-fitting clothing can reduce friction and irritation on the skin.
- Stress management: Managing stress through various techniques can potentially reduce the frequency of flare-ups.
It's important to remember that HS is a chronic condition, and finding the right treatment plan may take time. Working closely with a healthcare provider is essential for managing symptoms and improving quality of life.
Related Topics
What Causes Acne?
Acne primarily develops in adolescents during puberty. Androgens (male sex hormones) are the primary determinant of acne along with the presence of the bacteria P. acnes, and fatty acids (sebum) present in oil (sebaceous) glands.
Read moreStevens-Johnson Syndrome: Rare but Serious Skin Condition
While SJS is rare, it is a dangerous and potentially life-thretening disorder which affects the skin, mucous membranes, genitals, and eyes. It causes flu-like symptoms along with painful rash that spreads and blisters. If you or someone you know is exhibiting symptoms of SJS, seek medical attention immediately.
Read more