- Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects ovaries and the whole body.
- Symptoms include irregular periods, excess hair growth, thinning scalp hair, weight gain, mood changes, and difficulty conceiving.
- The exact cause of PCOS is not fully understood, but research suggests it is influenced by a combination of genetic, hormonal, and environmental factors.
- PCOS is one of the leading causes of infertility. This condition can make it harder to conceive due to the way it affects ovulation.
- For women who want to get pregnant treatment includes ovulation induction medications, metformin, and weight loss. For women who do not plan to get pregnant hormonal birth control, androgen lowering drugs, and metformin are used.
Overview
Polycystic ovary syndrome or PCOS is a health condition that affects the way hormones work in women. It is one of the most common hormonal disorders in those of reproductive age.
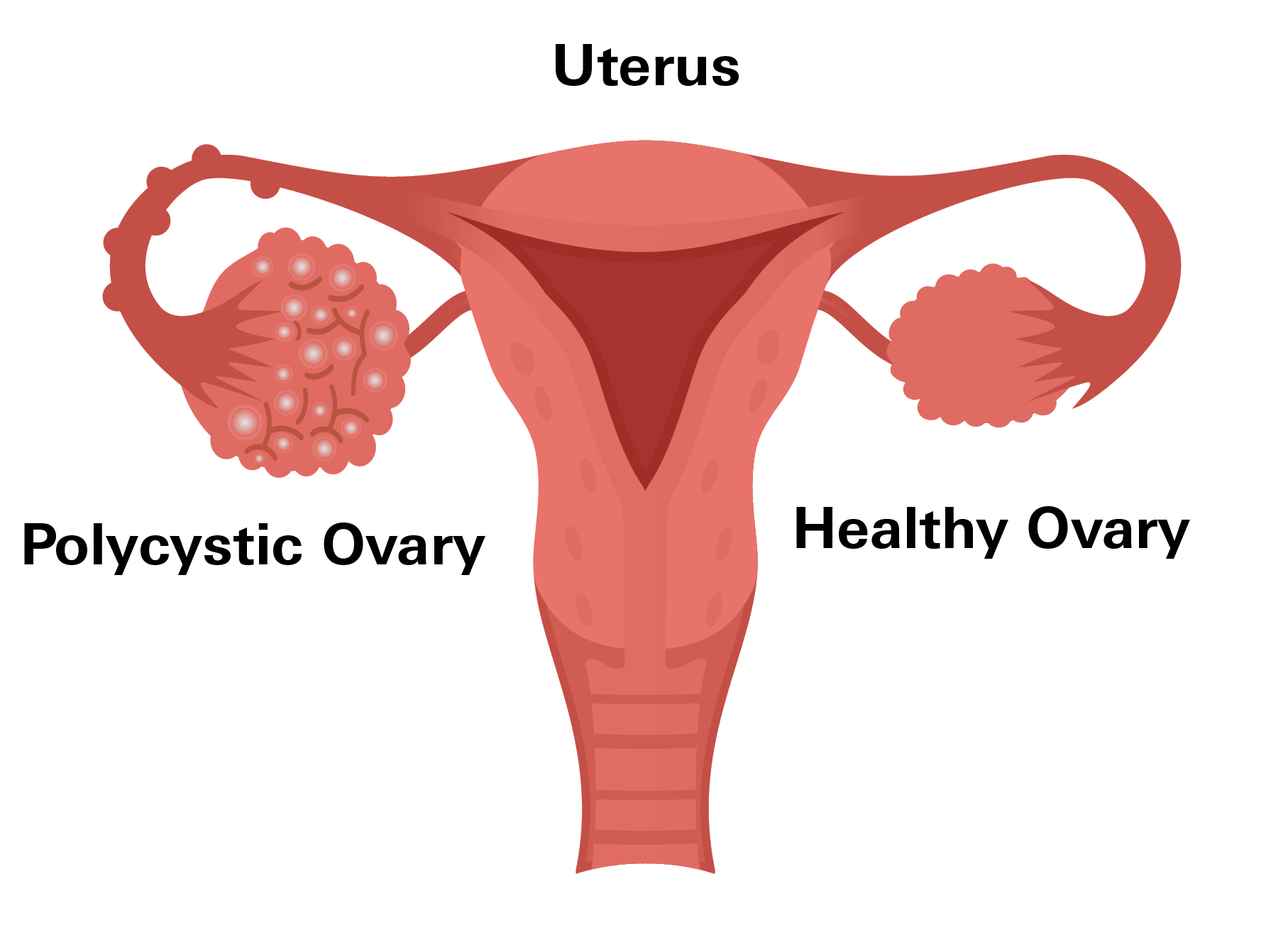
The term "polycystic" refers to small, fluid-filled sacs, called cysts, that can develop on the ovaries. However, not everyone with PCOS has these cysts, so the condition is more complex than its name suggests.
PCOS occurs because of hormonal imbalances, particularly involving androgens. Androgens are often called “male hormones,” but everyone produces them, regardless of gender. In PCOS, your body makes too many of these hormones, which can disrupt how the ovaries work. This can lead to irregular or missed periods, difficulty with ovulation, and symptoms such as acne, extra hair growth on your face or body, and thinning hair.
These hormonal changes can also affect other areas of health. For example, high androgen levels can interfere with how your body processes insulin, a hormone that controls blood sugar levels. This is why PCOS is linked to problems such as weight gain, insulin resistance, increasing the risk of type 2 diabetes, and other health issues.
Keep in mind that PCOS is not just about the ovaries, it’s a condition that can affect the whole body.
Prevalence
According to data from the U.S. Department of Health and Human Services (HHS), PCOS affects approximately 6% to 12% of women of reproductive age in the United States. This means that up to 5 million women in this group may be living with PCOS.
Studies also highlight that many cases of PCOS remain undiagnosed. Research estimates that about 50% of women with PCOS are unaware they have the condition, as its symptoms can vary widely and may overlap with other health issues.
Studies also found that PCOS is more frequently diagnosed in women with obesity, likely due to the exacerbating effects of excess weight on hormonal imbalances and insulin resistance. However, it is important to remember that PCOS affects women across all body types.
Symptoms
PCOS presents with a variety of signs and symptoms, and they may differ from one woman to another. Some of the most common indicators to look for include the following:
- Irregular periods: Missed, infrequent, or unpredictable menstrual cycles.
- Excess hair growth, also known as hirsutism: Noticeable hair on your face, chest, or back.
- Thinning scalp hair: Hair loss or reduced hair density on your head.
- Persistent acne: Especially along the jawline or on the back.
- Weight gain: Often concentrated around your abdomen.
- Darkened patches of skin: Commonly found on your neck, underarms, or groin.
- Difficulty conceiving: Caused by irregular or absent ovulation.
- Mood changes: Including anxiety or depression.
If you notice these signs in yourself, it’s recommended to speak with your doctor to explore potential underlying causes and options for management.
Causes
The exact cause of PCOS is not fully understood, but research suggests it is influenced by a combination of genetic, hormonal, and environmental factors.
Genetic
Studies indicate that PCOS often runs in families, suggesting a genetic component. If a close relative, such as a parent or sibling, has PCOS, the chances of developing it are higher. Researchers are still identifying specific genes that may be linked to the condition, but it is clear that hereditary factors play a role.
Hormone Imbalance
PCOS primarily develops due to imbalances in hormone levels. In addition to elevated androgens, women with PCOS often exhibit higher levels of luteinizing hormone (LH) and lower levels of follicle-stimulating hormone (FSH). This imbalance can affect the normal development and release of eggs from the ovaries. Some research emphasizes that the overproduction of LH, along with its interaction with other hormones such as insulin, may contribute to certain reproductive symptoms of PCOS.
Isulin Resistance
Insulin resistance plays a significant role in PCOS, affecting about 70% of women with the condition, even those who are not overweight. When your body’s cells become resistant to insulin, your pancreas compensates by producing more, leading to elevated insulin levels in your bloodstream. This excess insulin can stimulate your ovaries to produce more androgens, contributing to symptoms of PCOS. According to a study in The Journal of Clinical Endocrinology & Metabolism, high insulin levels are a major factor in many PCOS symptoms, including irregular periods and issues with ovulation.
Environments
Additionally, environmental factors, such as diet, lifestyle, and exposure to certain chemicals, may also contribute to the development of PCOS. Research also suggests that obesity can exacerbate the hormonal imbalances associated with PCOS, though it is not a direct cause.
Diagnosis
PCOS is diagnosed based on your medical history, symptoms, and specific tests. Generally, your gynecologist or an endocrinologist will be the specialist diagnosing and managing this condition.
To confirm PCOS, your doctor will consider criteria such as irregular periods, signs of elevated androgens, such as excess hair growth or acne, and the presence of cysts on your ovaries, which may be identified through an ultrasound.
Blood tests are often used to measure hormone levels and rule out other conditions with similar symptoms.
Additionally, your doctor might assess insulin resistance, cholesterol levels, and other markers to understand the broader effects of PCOS on your health.
PCOS and Pregnancy
PCOS is one of the leading causes of infertility, but it does not mean that pregnancy is impossible. Although, this condition can make it harder to conceive due to the way it affects ovulation.
Ovulation is the process where an egg is released from your ovary, making it available for fertilization. However, in women with PCOS, hormonal imbalances, particularly elevated androgens and insulin resistance, can prevent ovulation from occurring regularly. Without regular ovulation, it becomes more difficult to time conception.
Additionally, one of the reasons PCOS can cause infertility is the buildup of immature follicles in the ovaries. These follicles, which appear as small fluid-filled sacs on an ultrasound, do not mature enough to release an egg. This is often accompanied by irregular or missed periods, which further complicates conception.
Lifestyle changes, such as maintaining a healthy weight, eating a balanced diet, and staying physically active, can improve your body’s response to insulin and regulate hormones, which may restore ovulation in some cases.
For those who need additional support, medications are often available to help. Fertility treatments such as Clomid or letrozole are commonly used to stimulate ovulation. In some cases, in-vitro fertilization, commonly abbreviated as IVF, may be an option.
If you have PCOS and are planning to start a family, it is important to work closely with your doctor. They can help monitor your condition and recommend appropriate treatments.
Treatment
The treatment of PCOS varies based on your symptoms, overall health, and whether or not you are planning to get pregnant. While there is no cure for PCOS, various treatments can help manage symptoms, regulate hormonal imbalances, and reduce your risk of long-term complications.
Women Who Want to Get Pregnant
- Ovulation Induction Medications: Prescription medications such as clomiphene or letrozole are commonly used to stimulate ovulation. These treatments can help regulate your menstrual cycle and improve your chances of conception.
- Metformin: This medication improves insulin sensitivity and may help restore ovulation in some women with PCOS. Studies have shown that metformin can improve pregnancy rates when used alongside other fertility treatments.
- Weight Loss: Losing even a small amount of weight, 5% to 10% of your body weight, can significantly improve ovulation and increase your likelihood of pregnancy. Studies have found that weight loss improves both insulin resistance and reproductive function in women with PCOS.
Women Who Do Not Plan to Get Pregnant
- Hormonal Birth Control: Oral contraceptives, patches, or intrauterine devices (IUDs) can regulate menstrual cycles, reduce androgen levels, and manage symptoms such as acne and excess hair growth.
- Medications to Lower Androgens: Anti-androgen medications, such as spironolactone, can help reduce symptoms such as unwanted hair growth and scalp hair thinning. These medications work by blocking the effects of androgens in your body.
- Metformin: In addition to helping with ovulation, metformin can also help manage weight and insulin resistance, even in women who are not trying to conceive.
Weight Management
For both groups, weight loss is often recommended to manage symptoms and reduce your risk of complications. Lifestyle changes, including a balanced diet and regular exercise, are first-line recommendations.
Medications such as Ozempic (semaglutide), a GLP-1 receptor agonist, have gained attention for their effectiveness in promoting weight loss. Clinical trials have found that semaglutide helped patients lose an average of 15% of their body weight, which can improve symptoms and health in PCOS.
Prevention
Currently, there is no way to prevent PCOS. However, certain lifestyle choices may help reduce the severity of symptoms or lower your risk of developing complications associated with the condition.
Maintaining a balanced diet, regular physical activity, and managing a healthy weight can improve insulin sensitivity and hormonal balance, which are central to PCOS. While these measures cannot entirely prevent PCOS, they play a significant role in its management and can help minimize its impact on your health.
If you are concerned about your risk, especially if you have a family history of PCOS, discussing preventive care and monitoring with your doctor can be helpful.
Related Topics
8 Signs You Could Have Polycystic Ovary Syndrome
PCOS is primarily caused by an imbalance of hormones, specifically high levels of androgens (male hormones) and insulin. This hormonal imbalance disrupts the normal functioning of the ovaries.
Read moreWhat You Need to Know About Endometriosis?
Endometriosis is a painful, chronic condition defined by the presence of tissue similar to the uterine lining (endometrium) growing outside the uterus.
Read moreManaging Endometriosis: Navigating the Path to Diagnosis and Treatment
Endometriosis is a significant medical concern due to its widespread prevalence, impact on the lives of biological women, diagnostic challenges, association with infertility, ongoing research needs, and the importance of advocacy and support.
Read moreQuestions About Dysmenorrhea
Dysmenorrhea is the term used to describe very painful menstrual periods. Most people with periods experience some level of discomfort before and/or during their period. For some people, this pain and discomfort is beyond what is considered “normal”, to the point where it can be debilitating.
Read more