- Skin cancer occurs when skin cells grow abnormally and out of control. This happens due to damage caused by ultraviolet (UV) radiation from the sun or tanning beds.
- There are 3 main types:
- Basal cell carcinoma (BCC): Most common type. Appears as glossy or waxy bumps on face and neck.
- Squamous cell carcinoma (SCC): Rough, scaly patches or red, firm bumps on scalp, ears, lips, or hands. It has a greater potential to develop on mucous membranes, such as your lips, and may present as a persistent sore or rough patch in these areas.
- Melanoma: Least common but most dangerous type. Often starts in an existing mole or appears as a new dark spot on your skin.
- Some risk factors include fair skin, weakened immune system, old age, and skin conditions like actinic keratosis.
- Diagnosis is through a visual inspection and a biopsy. Once it's confirmed, staging is performed to determine how far the cancer has spread.
- Treatment options include surgery, radio therapy for challenging areas, immunotherapy for advanced melanoma, or non-invasive therapy like cryotherapy (freezing) and photodynamic (light) therapy.
- You can minimize the risk by limiting sun exposure, wearing protective clothes, and using sunscreen.
Overview
Skin cancer occurs when skin cells grow abnormally and out of control. This happens due to damage caused by ultraviolet (UV) radiation from the sun or tanning beds. It can appear in many forms and may show up as new growths, changes in existing moles, or wounds that do not heal. Skin cancer varies in how it looks and behaves, depending on the type.
There are 3 main types of skin cancer:
-
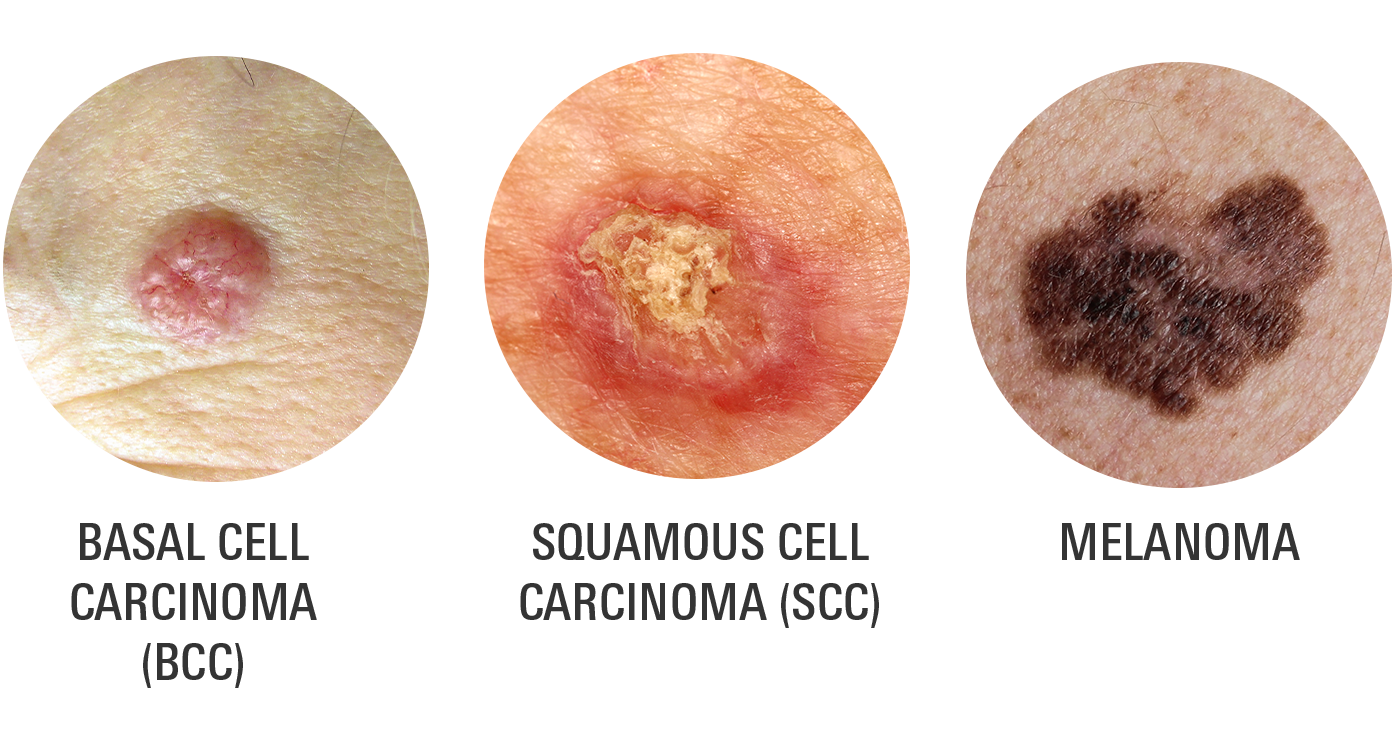
Basal cell carcinoma (BCC)
This is the most common type of skin cancer. It often appears as glossy or waxy bumps, primarily on sun-exposed areas such as your face and neck. BCC grows slowly and rarely spreads to other parts of your body, but it can still cause damage to nearby tissues if untreated.
In some cases, BCC may appear as a flat, flesh-colored, or brown scar-like area. - Squamous cell carcinoma (SCC)
SCC often appears as rough, scaly patches or red, firm bumps. It may also appear as an open sore that bleeds or crusts over. This type of skin cancer usually develops in areas exposed to the sun, such as your scalp, ears, lips, or hands.
Unlike BCC, SCC has a higher chance of spreading to deeper tissues or other areas of your body if it is not treated right away. - Melanoma
Melanoma is the least common but the most serious and dangerous type of skin cancer. It often starts in an existing mole or appears as a new dark spot on your skin. It is identified by its irregular shape, uneven color, and changes over time.
Melanoma can be black, brown, red, or even skin-colored, and it can spread quickly to other parts of your body, making early detection important.
To differentiate between these types of skin cancer, the ABCDE rule is used as a helpful guide:
- Asymmetry: If you draw a line through the middle of a spot, the 2 halves don’t match.
- Border: The edges of the spot are uneven or blurred.
- Color: There are multiple shades of brown, black, red, or white within the same spot.
- Diameter: The spot is larger than 6mm, about the size of a pencil eraser.
- Evolving: The spot changes in size, shape, or color over time or starts to itch, bleed, or feel painful.
It is important to note that skin cancer may sometimes be tricky to recognize because not all cases follow the same patterns.
Prevalence
Skin cancer is the most common form of cancer in the United States.
- Basal cell carcinoma is the most common type, with an estimated 3.6 million cases diagnosed annually
- Squamous cell carcinoma follows, with approximately 1.8 million cases each year.
- Melanoma, though less common, is more serious; in 2025, about 104,960 new cases are expected, with an estimated 8,430 resulting in death.
That being said, 1 in 5 Americans is projected to develop skin cancer by age 70.
Symptoms
Skin cancer can present differently depending on the type, making it important to recognize the specific signs and symptoms associated with each.
Basal Cell Carcinoma (BCC)
- BCC develops in areas with frequent sun exposure: face, ears, neck, and scalp.
- A hallmark is its ability to appear in different forms, which may be mistaken for benign skin conditions.
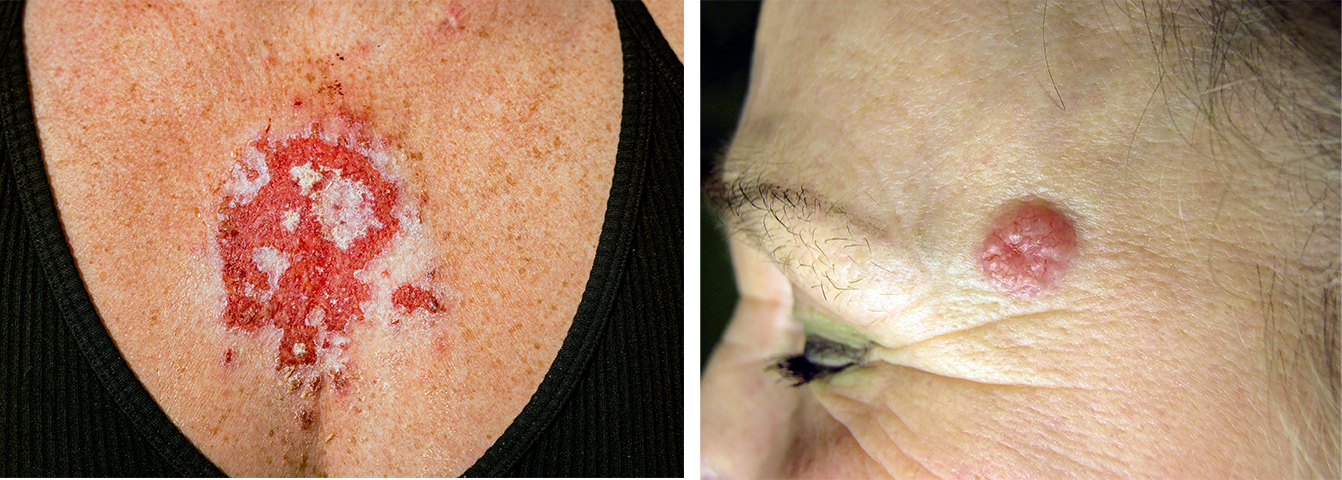
- Some BCCs can take on a pink or red tone with fine blood vessels visible on the surface. Another potential form is a white, scar-like area that feels waxy or firm to the touch.
- Over time, untreated BCC lesions can grow deeper, potentially causing disfigurement.
Squamous Cell Carcinoma (SCC)

- SCC can vary in appearance. Beyond the classic scaly or crusted patch, it may resemble a thickened area of skin or a persistent, raised sore.
- It is common for SCC to develop a hardened, wart-like texture, which sets it apart from other skin lesions. The lesions can ulcerate, meaning they break open and form a sore, sometimes with a raised border.
- Unlike BCC, SCC has a greater potential to develop on mucous membranes, such as your lips, and may present as a persistent sore or rough patch in these areas. It is also more likely to grow aggressively and spread, especially if it leads to scars or wounds.
Melanoma

- Melanoma is distinctive because it can resemble harmless moles or freckles.
- In addition to the classic ABCDE characteristics, melanomas can sometimes be colorless or present as pink, red, or flesh-toned lesions, which makes them harder to identify.
- They may also develop in unusual places, such as the soles of your feet, under your nails, or on your palms, especially in those with darker skin tones.
- Changes in texture, such as becoming rougher or harder, and symptoms, including itching, tenderness, or bleeding, are additional warning signs.
- Melanoma can also occasionally spread under the surface of your skin without forming a visible lesion.
Causes
Skin cancer occurs when the DNA in skin cells is damaged, leading to abnormal and uncontrolled cell growth. This damage is often caused by UV radiation, but other factors can also contribute.
Sun Exposure
The leading cause is extended or intense exposure to UV rays from sunlight. These rays penetrate your skin and damage its DNA, especially in areas frequently exposed, such as your face, neck, and hands.
It is important to note that artificial UV radiation from tanning beds also increases your risk significantly, particularly for younger patients. Both natural and artificial UV radiation can lead to all types of skin cancer.
The risk of skin cancer is also higher in those with fair skin, freckles, or light-colored eyes, as their skin has less melanin. Melanin provides some protection by absorbing and reducing UV damage.
Weakened Immune System
A weakened immune system, such as in patients going through organ transplants, living with HIV, or taking immunosuppressive medications, also reduces the body's ability to repair damaged skin cells and fight off abnormal growths, further increasing your risk.
Age
Age can affect the development of skin cancer as the effects of UV exposure build up over time. Skin cancer can also occur in younger patients, particularly if there has been significant sun damage earlier in life. For example, severe sunburns during childhood or adolescence can have long-term effects on the skin.
Medical Conditions
Other contributing factors include precancerous skin conditions such as actinic keratosis, which are rough, scaly patches caused by long-term sun damage. These can progress to skin cancer if untreated.
Diagnosis
Skin cancer diagnosis begins with a thorough exam of your skin by your doctor, often your dermatologist on suspicious lesions or spots. If the appearance raises concern, further testing, such as a biopsy, is performed to confirm the presence of cancer cells and determine the type of skin cancer.
Skin Exam
The process starts with a visual inspection. Your dermatologist uses a dermatoscope, a magnifying tool, to assess your lesion's features, including size, shape, border, color, and texture. They look for irregularities that may suggest cancer.
Skin Biopsy
If a lesion appears suspicious, a biopsy is the definitive step to confirm the diagnosis. A small piece of skin, or the entire lesion, is removed and analyzed under a microscope. The biopsy not only confirms whether cancer is present but also identifies the type.
Staging
Once a diagnosis is confirmed, staging is performed to determine how far the cancer has spread. Staging is particularly important for melanoma and advanced squamous cell carcinoma. It helps guide treatment decisions and provides insight into prognosis.
- Stage 0: The cancer is localized to the top layer of the skin (epidermis) and has not spread to deeper layers or other tissues.
- Stage I: The cancer is small (usually less than 2cm across for non-melanoma skin cancers) and has not spread beyond the site of origin. It may extend into the dermis but has not reached nearby lymph nodes or other tissues.
- Stage II: The cancer is larger or has certain features (such as rapid growth or ulceration) but remains confined to your skin and has not spread to lymph nodes or other organs.
- Stage III: The cancer has spread to nearby lymph nodes or tissues but has not reached distant parts of your body. This stage often requires more aggressive treatment..
- Stage IV: The cancer has metastasized, meaning it has spread to distant parts of your body, such as the lungs, liver, or bones. This stage is rare for basal cell carcinoma but more common for melanoma and advanced squamous cell carcinoma.
In some cases, additional diagnostic tools are used to stage cancer, particularly if there is concern about its spread. For example, CT scans or MRI scans can help detect cancer in lymph nodes or distant organs.
Risk Factors
Although anyone can develop skin cancer, certain factors can significantly increase the likelihood of its occurrence. Major risk factors include the following:
- Prolonged UV exposure (sunlight or tanning beds)
- History of childhood sunburns
- Fair skin, light-colored eyes, and red or blonde hair
- Genetic conditions affecting skin or DNA repair
- Immunosuppressive conditions or medications
- Chronic wounds, scars, or long-term inflammation
- Personal history of skin cancer or precancerous lesions
- Advancing age and cumulative UV damage
- Men are more likely to develop basal and squamous cell carcinoma, possibly due to more frequent outdoor occupations and less use of sun protection.
- Women have a higher likelihood of developing melanoma on their legs, which may be due to differences in clothing choices and sun exposure patterns.
- Smoking has been linked to an increased risk of squamous cell carcinoma, especially on your lips
Treatment
Skin cancer treatment depends on the type, stage, size, and location of the cancer, as well as your overall health.
Surgery
Surgery is the most common and effective treatment for many types of skin cancer, particularly in its early stages.
Excisional surgery involves removing the cancer along with a small margin of healthy tissue to make sure that all cancer cells are taken out. For more complex cases, especially in sensitive areas such as your face, Mohs surgery is often used. This technique removes thin layers of tissue and examines them under a microscope during the procedure, minimizing healthy tissue loss while providing complete cancer removal.
Curettage and electrodesiccation: These procedures are suitable for smaller and superficial areas. They involve scraping away the cancer followed by applying heat or electricity to destroy remaining cells.
Radiation Therapy
Radiation therapy is another option, particularly for cases where surgery is not appropriate or when the cancer is located in challenging areas. High-energy beams are directed at the cancer to destroy cells. Radiation may also be used after surgery to reduce the risk of recurrence, particularly for advanced SCC or melanoma.
Chemotherapy can be used for skin cancers that have spread or are difficult to treat with localized methods.
- Systemic chemotherapy: Administered through the bloodstream, primarily for advanced melanoma or SCC.
- Topical chemotherapy: Applied directly to the skin (e.g., creams containing fluorouracil).
Immunotherapy
Immunotherapy is particularly effective for advanced melanoma. This treatment helps your immune system recognize and attack cancer cells.
Topical immunotherapy: Creams like imiquimod stimulate an immune response against localized cancers.
Cryotherapy
Cryotherapy, or freezing cancer cells with liquid nitrogen, is a non-invasive option for small or superficial skin cancers, such as actinic keratosis or early BCC. The frozen cells die and naturally slough off as the skin heals.
Photodynamic Therapy (PDT)
PDT offers another non-invasive treatment for superficial skin cancers. A photosensitizing agent is applied to your skin and then activated with a specific type of light, which destroys the cancer cells. This treatment can be beneficial for patients who cannot or prefer not to undergo surgery.
Combination Treatments
In some cases, a combination of treatments may be recommended, especially for advanced or recurrent skin cancers.
Prevention
Protecting your skin from harmful UV radiation is key to preventing skin cancer.
- Limit sun exposure: Minimize time spent in the sun, especially during peak hours (10 a.m. - 4 p.m.).
- Wear protective clothing: Long sleeves, wide-brimmed hats, UV-blocking sunglasses.
- Use sunscreen: Apply a broad-spectrum sunscreen with an SPF of 30 or higher daily, even on cloudy days. Reapply every 2 hours, especially after swimming.
- Avoid tanning beds: Tanning beds expose your skin to high levels of UV radiation.
Paying attention to skin health is particularly important for those with a family history of skin cancer. If you think you may have skin cancer, contact your dermatologist or healthcare provider for an evaluation. A doctor can assess any unusual lesions or spots and perform a biopsy if needed to confirm whether cancer is present.
Remember that early detection often leads to simpler and more effective treatments. Avoid self- diagnosing or delaying medical care, as untreated skin cancer may grow or spread.
Related Topics
What is Imiquimod cream used for?
If you're dealing with skin conditions like actinic keratosis, superficial basal cell carcinoma, or genital warts, Imiquimod may be the treatment option you've been looking for.
Read moreHow Fluorouracil Cream Can Help Treat Skin Cancer and Precancerous Spots
Fluorouracil cream is a commonly prescribed medication often categorized as a chemotherapy treatment. It's used to treat various skin conditions, including actinic keratosis and certain types of skin cancer, such as superficial basal cell carcinoma.
Read moreFluorouracil Cream for Actinic Keratoses
Fluorouracil cream is a topical medication commonly used in dermatology to treat specific skin conditions that are associated with cancer. This cream is an FDA-approved treatment primarily used for addressing superficial basal cell carcinoma (SBCC) and actinic keratoses.
Read more