- Allergic rhinitis, commonly known as hay fever, is an allergic reaction that causes inflammation of the nasal passages.
- Common symptoms include sneezing, itching, nasal congestion, and a runny nose.
- The main causes of allergic rhinitis are pollen, dust mites, mold spores, pet dander, and certain foods.
- Treatment options include allergen avoidance, medications (antihistamines, nasal corticosteroids, etc.), and immunotherapy (allergy shots or sublingual tablets).
Overview
Allergies, also referred to as allergic rhinitis or hay fever, is a medical condition in which your immune system reacts to a foreign substance that is normally harmless to most individuals.
These foreign substances, referred to as allergens, can be anything from pollen and dust mites to pet dander, medications, and/or insects.
When a person with allergic rhinitis comes into contact with these allergens, their immune system overreacts and releases chemicals such as histamine, leading to the characteristic symptoms of sneezing, itching, nasal congestion, and a runny nose.
Other factors that may contribute to the development of allergies include diet, stress, and changes in gut microbiota.
Some allergy symptoms can also be caused by other conditions, including colds or sinus infections. If you're unsure whether your symptoms are due to allergies or a cold, read 'Allergy or Cold'.
Prevalence
Seasonal allergies are a common form of allergies in the United States. They occur during specific times of the year when certain plants release pollen into the air. These allergies affect a significant portion of the population, with estimates suggesting that around 8% to 10% of Americans experience symptoms of seasonal allergies.
Allergic rhinitis are a common form of allergies in the United States, affecting a significant portion of the population. According to the Asthma and Allergy Foundation of America, around 8% of adults and 9% of children in the US experience hay fever symptoms.
Allergy Season
Depending on the allergen and the area, the allergy season can change. The peak allergy season typically coincides with the time of year when plants release pollen into the atmosphere.
For instance, tree pollen is most prevalent in the spring in the United States, often beginning in February or March and lasting until May. The late spring and summer, often beginning in May and lasting until July or August, are the seasons when grass pollen is most prevalent. Ragweed pollen is particularly prevalent in the fall, typically beginning in August and continuing until fall.
Yet, elements like weather patterns and climate changes can affect the timing and intensity of allergy season. Allergies can also be brought on year-round by indoor allergens including dust mites, pet dander, and mold.
Those with known allergies need to be aware of their symptoms and triggers and work with their doctor to create a management plan that includes avoiding triggers, taking medication, and, if necessary, seeking emergency care.
Symptoms
Signs and symptoms of allergies can vary depending on the type of allergen and the severity of your reaction.
Common signs and symptoms include the following:
- Sneezing
- Runny or stuffy nose
- Itchy or watery eyes
- Redness or swelling of the skin
- Hives or rashes
- Coughing or wheezing
- Shortness of breath
- Abdominal pain or cramping
- Diarrhea or vomiting
In severe cases, allergies can lead to what’s called anaphylaxis, which is a potentially life- threatening reaction that can cause the following:
- Difficulty breathing
- Swelling of your face, throat, and/or tongue
- Increased heartbeat
- Dizziness and/or fainting
- Confusion and/or disorientation
If you experience any of these symptoms after exposure to an allergen, seek emergency medical care immediately.
Triggers
Allergy triggers can differ from person to person depending on the type of allergen and your sensitivity.
Some common allergy triggers may include the following:
- Pollen
Pollen from trees, grasses, and weeds is a common cause of seasonal allergic rhinitis. Different plants produce pollen at different times of the year, so symptoms may occur during specific seasons.
- Dust mites
Dust mites are microscopic organisms that live in dust and thrive in warm and humid environments. Their droppings and decomposed bodies contain allergenic proteins that can trigger allergic reactions.
- Mold spores
Mold spores are airborne fungal particles. They can be found both indoors and outdoors, particularly in damp and humid environments. Inhalation of mold spores can cause allergic rhinitis symptoms.
- Pet dander
Proteins found in the skin cells, saliva, and urine of animals, such as cats, dogs, and rodents, can cause allergic reactions in sensitive individuals.
- Cockroaches
Cockroach debris and droppings can trigger allergic rhinitis symptoms, especially in urban areas where cockroach infestations are more common.
- Certain foods
In some cases, specific foods can cause allergic rhinitis symptoms. This condition, known as oral allergy syndrome, typically occurs when certain fresh fruits, vegetables, or nuts cross-react with pollen allergens. For example, eating an apple may trigger symptoms in someone with birch pollen allergy.
- Occupational allergens
People working in certain occupations may be exposed to allergens that cause allergic rhinitis. These include chemicals, dust, or biological agents encountered in industries like farming, woodworking, hairdressing, or healthcare.
It's important to note that allergic rhinitis is an allergic condition and is not caused by viruses or bacteria. Additionally, genetics and family history play a role in determining a person's susceptibility to allergic rhinitis. If you suspect you have allergic rhinitis, it is recommended to consult with a healthcare professional for proper diagnosis and management of your symptoms.
Diagnosis
Allergies are typically diagnosed based on a combination of medical history, physical exam, and/ or diagnostic tests.
Some common methods used to diagnose allergies include the following:
- Medical history: Your healthcare provider will ask about your symptoms, including the timing and duration of your symptoms, and any triggers that may be causing your allergic reaction.
- Physical exam: Your doctor will examine your skin, eyes, nose, and/or throat for signs of an allergic reaction, including hives, swelling, and/or redness.
- Skin tests: Skin tests involve placing a small amount of allergen on your skin, typically on your arm or back, and then pricking or scratching your skin to allow the allergen to enter. If you happen to be allergic to the particular substance, then this results in a red, raised bump known as a wheal will appear within 15 to 20 minutes.
- Blood tests: Blood tests can measure the levels of IgE antibodies in your blood, which can help identify specific allergens that may be triggering your symptoms.
Diagnosing allergies can be difficult, but it's important to work closely with your doctor or allergist to identify the specific allergen and develop an effective treatment plan.
Treatment
Selecting the appropriate medication treatment depends on the severity of your condition and your symptoms.
Intranasal Steroids
Intranasal steroids are considered the first-line treatment for chronic or long-term moderate-to-severe nasal congestion. These medications work by reducing inflammation in the nasal passages, effectively alleviating symptoms such as sneezing, runny nose, and congestion. Relief from symptoms may take up to one week after starting treatment.
- Budesonide (Rhinocort Allergy OTC): 1 spray per nostril daily. This is the preferred nasal steroid for pregnant women.
- Fluticasone (Flonase Sensimist Allergy Relief): 1-2 sprays per nostril daily.
- Nasacort Allergy 24HR OTC: 1-2 sprays per nostril daily (for adults and children 6 years and older).
- Flunisolide: 2 sprays per nostril twice or three times a day.
- Mometasone (Nasonex): 2 sprays per nostril daily.
Common side effects include headache, dry nose, nosebleeds, unpleasant taste, localized infection.
Oral Antihistamines
Oral antihistamines are used to manage mild to moderate, intermittent allergy symptoms, such as itchy or red eyes. They are effective at reducing itching, sneezing, and runny nose, though they have minimal impact on nasal congestion.
- First-Generation Oral Antihistamines
- Diphenhydramine HCL (Benadryl): 25-50 mg taken orally every 4 to 6 hours. For children aged 6-11 years: 12.5-25 mg every 4 to 6 hours.
- Chlorpheniramine: IR (Immediate-Release): 4 mg every 4 to 6 hours. ER (Extended-Release): 12 mg every 12 hours.
- Common side effects include sleepness, cognitive impairment, dry mouth, blurred vision, urinary retention, constipation, seizure (at high doses), increased heart rate (at high doses)
- Second-Generation Oral Antihistamines
- Cetirizine (Zyrtec): 5-10 mg taken daily. For children aged 2-5 years: 2.5-5 mg daily.
- Levocetirizine (Xyzal Allergy 24HR OTC): 5 mg taken every night before bed.
- Fexofenadine (Allegra): 60 mg twice a day or 180 mg daily. Must be taken with water, not juice, to ensure proper absorption.
- Loratadine (Claritin): 10 mg daily or 5 mg twice a day.
Common side effects include sleepness and headache.
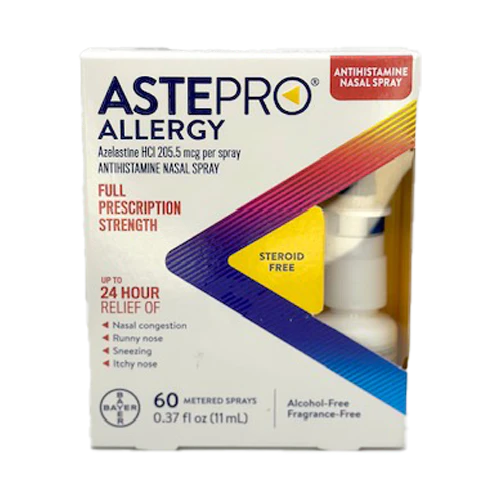
Intranasal Antihistamines
Intranasal antihistamines help alleviate nasal congestion and can be used in combination with intranasal steroids for enhanced effectiveness.
- Azelastine + Fluticasone (Dymista): 1-2 sprays per nostril twice a day.
- Olopatadine (Patanase): 2 sprays per nostril twice a day.
Common side effects include bitter taste, headache, nasal irritation, nosebleeds, sinus pain.
Decongestants
Decongestants are effective in reducing sinus and nasal congestion.
- Phenylephrine PE (Sudafed PE): 10 mg taken every 4 hours as needed.
- Pseudoephedrine (Sudafed): 60 mg every 4-6 hours as needed, 120 mg every 12 hours, or 240 mg daily.
Note: Due to its potential use in methamphetamine production, pseudoephedrine has restricted distribution and is only available behind the counter.
Common side effects include increased heart rate, palpitations, elevated blood pressure, anxiety, tremors, insomnia, nervousness, restlessness, dizziness, headache, loss of appetite.
Topical (Intranasal) Decongestants
- Oxymetazoline 0.05% (Afrin): 2-3 sprays per nostril every 12 hours as needed.
- Phenylephrine (various concentrations): 2-3 sprays per nostril every 4 hours as needed.
Common side effects include nasal stinging, burning, and/or dryness, sneezing, rhinitis medicamentosa (rebound congestion if used longer than 3 days).
Immunotherapy
Allergen immunotherapy, commonly known as allergy shots, helps develop your tolerance to allergens, potentially reducing or eliminating symptoms over time. This involves regular administration of gradually increasing doses of allergens until a maintenance level is reached.
Prevention
For some, allergies can be prevented or their severity reduced by taking certain steps. Some steps that can be taken to help prevent your allergies may include the following:
- Avoid allergens: The best way to prevent allergies is to avoid exposure to the allergen.
- Practice good hygiene: Regular hand-washing and keeping a clean environment can help reduce exposure to allergens, including dust mites and pet dander
- Breastfeed: Breastfeeding may help reduce the risk of developing allergies in infants.
- Introduce solid foods slowly: When introducing solid foods to infants, it's important to introduce them one at a time and in small amounts to help identify any potential food allergies.
- Manage stress: High levels of stress can weaken your immune system and make allergy symptoms worse. Practicing stress-management techniques, such as meditation or yoga, can help reduce the impact of stress on your body.
- Immunotherapy: Immunotherapy can help desensitize your immune system to specific allergens and reduce the severity of symptoms over time.
It's important to keep in mind that not all allergies can be prevented, and some may be more prone to developing allergies due to genetic factors. However, taking the appropriate steps to reduce exposure to allergens and manage symptoms can help improve the quality of life for those with allergies.
Allergy or Cold
You likely have seasonal allergies if you frequently experience unexpected "colds" that occur around the same time every year. Although allergies and colds share similar symptoms, they are different diseases.
Read moreThe Atopic Triad: Asthma, Eczema, and Allergic Rhinitis
It has been observed that these three conditions often coexist within individuals and families. For example, if your mother has one of these atopic conditions, you have a 50% chance of developing any one of the three. If both parents have an atopic condition, the risk increases to 80%.
Read moreWhat to Use for Allergies
Allergies are caused by an over-reactive immune system to substances that are typically harmless, like cat hair or grass pollen. Your body mistakenly perceives these substances as threats, triggering allergic reactions. They are a wide array of allergies, each with distinct causes and associated symptoms or responses.
Read more