- Multiple Sclerosis (MS) is an autoimmune disease where the immune system attacks the myelin sheath, the protective covering of nerve fibers, leading to disruptions in nerve signal transmission.
- MS symptoms can vary widely, including fatigue, muscle weakness, difficulty with coordination and balance, vision problems, and cognitive impairments. The severity and progression of symptoms differ from person to person.
- MS is typically diagnosed between the ages of 20 and 40, with women being more frequently affected than men. Diagnosis is based on a combination of medical history, neurological exams, and imaging tests like MRI.
- While there is no cure for MS, treatments are available to manage symptoms, slow disease progression, and improve quality of life. These include disease-modifying therapies (DMTs), physical therapy, and lifestyle modifications.
Overview
Multiple sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system (CNS), which includes the brain and spinal cord. In MS, the immune system mistakenly attacks the myelin sheath, a protective layer that surrounds nerve fibers. This damage can disrupt the communication between the brain and other parts of the body, leading to a wide range of symptoms.
MS is a complex disorder with a variety of causes and manifestations. While the exact cause of MS remains unknown, it is believed to be a combination of genetic and environmental factors. The disease can affect people of all ages, but most often develops between the ages of 20 and 40.
Myelin
The CNS is the communication center of your body, receiving information from your senses such as sight, smell, sound, and touch. This information is used to control your body's movement, sensation, perception, thought, and memory.
When MS attacks and damages the CNS (myelin sheath on nerve cells), it can lead to various symptoms including numbness, weakness, vision issues, and difficulty with coordination and balance. MS is believed to be an autoimmune disease where the immune system mistakenly attacks healthy tissue (myelin sheath) in the CNS.
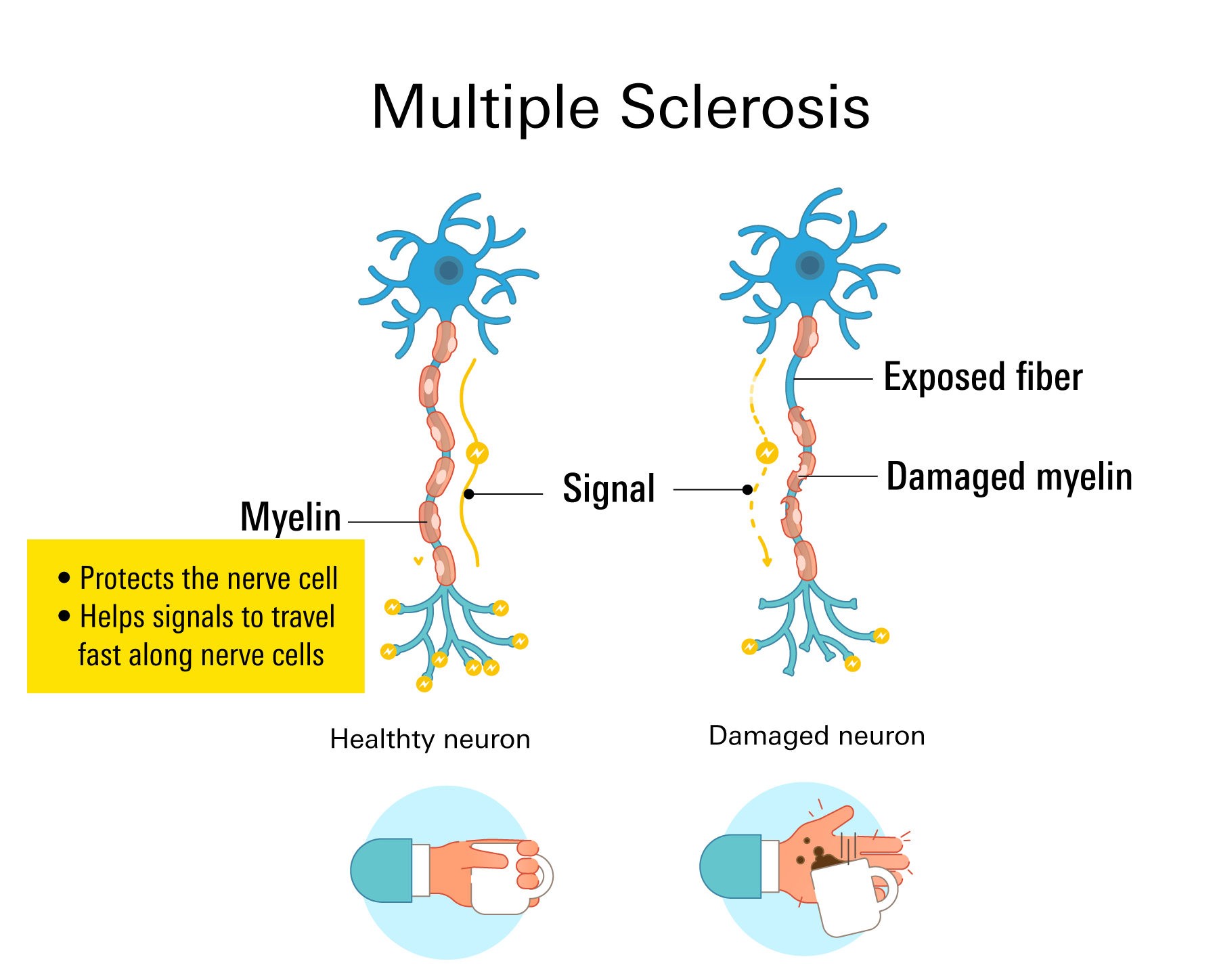
Myelin is the protective sheath that surrounds nerve fibers. It affects how fast electrical signals travel through nerve cells. When myelin is damaged, it impairs your brain-to-body interaction (communication). Sclerosis is a type of scar tissue created by myelin loss. This type of nerve injury prevents the nerves from carrying electrical impulses to and from your brain.
Multiple sclerosis a long-term unpredictable condition that may eventually cause nerve fiber degeneration or irreversible injury. Although MS is unpredictable and incurable, there are treatment options that accelerate the recovery process following attacks, change the course of the condition, and control symptoms.
Prevalence
The United States does not mandate the reporting or tracking of MS prevalence, which has made obtaining accurate estimates challenging. According to a 2019 study funded by the National MS Society, nearly 1 million people in the U.S. have been diagnosed with MS, a figure more than double that of previous estimates.
On a global scale, MS organizations estimate that approximately 2.3 million people were living with MS, a number that has since increased to 2.9 million by 2023, according to the Atlas of MS.
Demographic Insights
A detailed analysis in May 2023 examined health insurance claims from 96 million adults across the U.S. The study found that for every 1,000 people in the U.S., the prevalence of MS is:
- About 4 white people who are not Hispanic/Latinx
- About 3 Black people who are not Hispanic/Latinx
- About 1.5 Hispanic/Latinx people
- About 2 people of other races, including Asians, Native Americans, Alaska Natives, and people of several races or unknown race
The study could not definitively determine if MS is increasing. However, scientists speculate that the higher numbers may be due to longer life spans, improved diagnostic methods, and better representation of previously underrepresented groups.
Symptoms
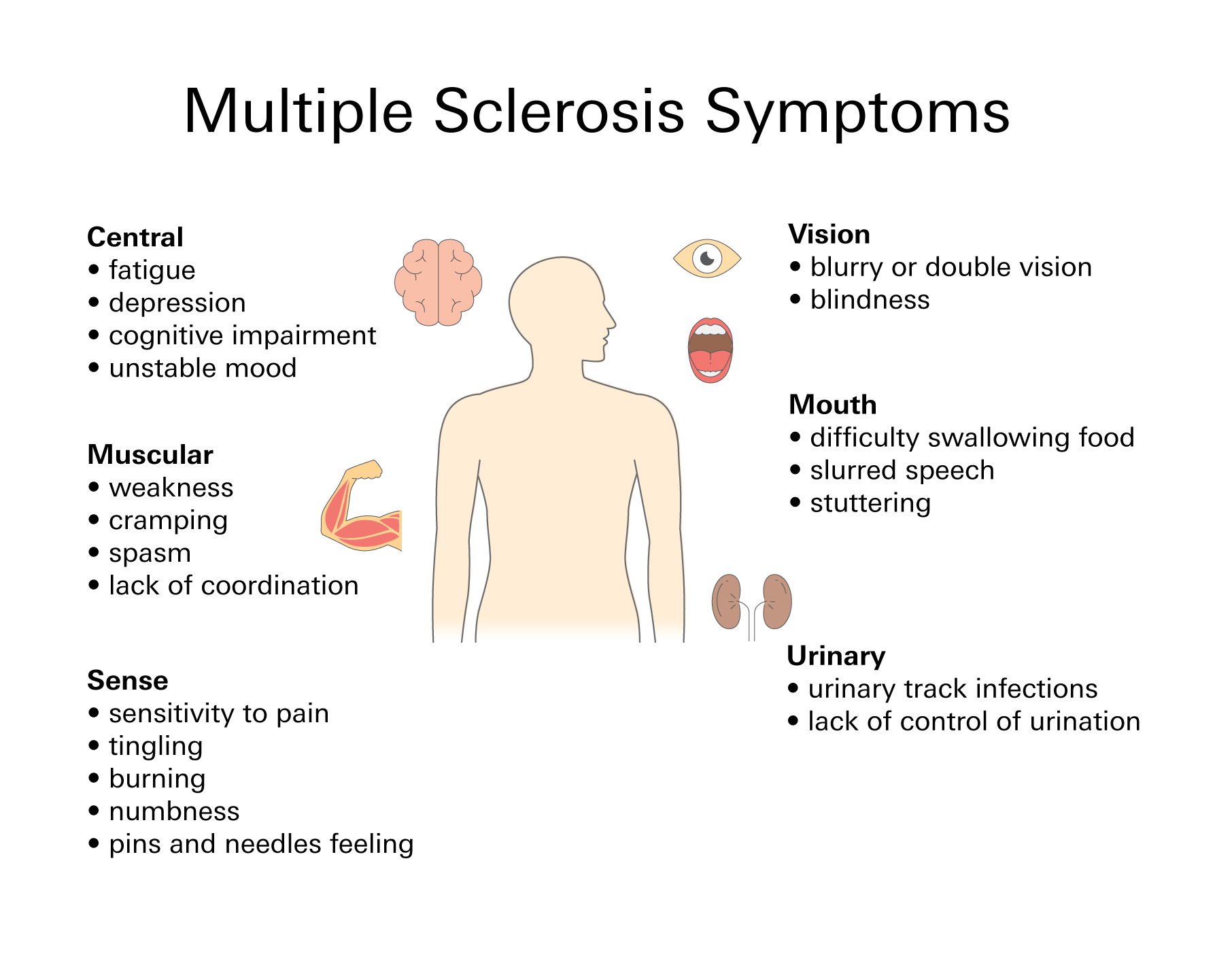
Common signs and symptoms of multiple sclerosis include the following:
- A tingling sensation
- Fatigue
- Slurred speech
- Changes in your mood, including depression
- Red or green color distortion
- Dizziness
- Vertigo
- Inability to walk or an unsteady stride
- Numbness, prickling, or pins & needles
- Vision problems
- Muscle weakness
- Tremor
- Heat sensitivity
Deterioration of cognitive function or issues with thinking is present in approximately 50% of individuals with multiple sclerosis. Your doctor may only discover these problems after conducting extensive tests. The difficulties might be with:
- Memory
- Focusing or concentration
- Faulty judgment
Primary: signs and symptoms are the outcomes of myelin damage.
- Loss of feeling or a feeling numb
- Shaking or tremors
- Loss of balance
- Vision problems, including loss of vision
- Pain or weakness
- Paralysis
- Issues with your bladder
Secondary: caused by your primary symptoms.
- Weakness, muscle imbalances, and reduced bone density can be brought on by inactivity.
- Urinary tract infections (UTIs) can occur often as a result of bladder issues.
- Incontinence or lack of control of urination can result from muscle impairment
- Bedsores can result from paralysis.
Tertiary: psychological and social concerns
- Depression
- Decreased quality of life
- If you lose the ability to drive or walk, you risk losing your job
Although multiple sclerosis can occur in both men and women, its more common in women. However, men frequently have the poorest prognosis and might have a more progressive version of the illness compared to women.
Types
There are 4 main forms of multiple sclerosis, and they include:
- Clinically isolated syndrome (CIS): A single, initial episode caused by inflammation in the central nervous system. To be identified as CIS, the symptoms must persist for at least 24 hours. Many people who experience CIS never get MS, but for some this initial episode is an early sign for developing MS.
- Relapse-remitting MS (RRMS): The most common type of MS. Approximately 85% of multiple sclerosis cases are RRMS. It is identified by clearly defined attacks (relapses) followed by period of recovery (remission). Relapses can show new or worsening symptoms.
- Primary progressive MS (PPMS): 15% of individuals with multiple sclerosis have symptoms that gradually get worse over time without remissions or relapses. Many individuals could go through stable times as well as moments when symptoms become worse before getting better.
- Secondary progressive MS (SPMS): For many people this type of MS comes after RRMS (release-remitting MS). With SPMS individuals initially go through periods of remission and relapse, then the illness starts to advance gradually.
Risk factors
MS is an autoimmune disorder and the exact cause is unknown. Researchers believe that a combination of genetic, environment, and sex can increase the risk. Common risk factors to look out for with multiple sclerosis include the following:
- Sex—women are more likely to develop multiple sclerosis compared to men.
- Age—between the ages of 20 and 40, the majority of individuals with multiple sclerosis may get diagnosed.
- Vitamin D deficiency—multiple sclerosis is more prevalent in individuals who receive less direct sunlight, which your body needs to produce vitamin D. According to some researchers, your immune system may be impacted by low vitamin D levels.
- Infections—some studies have demonstrated a connection between multiple sclerosis risk and exposure to viruses such as Epstein-Barr virus (EBV) or mononucleosis. Mycoplasma pneumonia and the human herpes virus type 6 (HHV6) are 2 other viruses that might be involved.
- Smoking—multiple sclerosis seems to be more prone to develop among smokers. In comparison to non-smokers, they also frequently have greater lesions and brain atrophy.
Diagnosis
Unfortunately, there are no specific tests used to diagnose multiple sclerosis. To diagnose multiple sclerosis, specialists commonly exclude other illnesses that might cause comparable signs and symptoms, a process called a differential diagnosis.
Some ways multiple sclerosis may be diagnosed include the following:
- Blood test
Assists in ruling out conditions with symptoms similar to multiple sclerosis. Currently being developed are tests that are used to look for particular biomarkers linked to MS that may help with diagnosis. - MRI
Brain and spinal cord scans may detect lesions (areas of damage). Evoked potential testing may be advised by your neurologist if the results of these tests are unclear. - <>Evoked potential test
This test captures the electrical impulses that your nervous system generates in reaction to stimuli. During this exam, nerves in your arms or legs are stimulated with brief electrical impulses as you observe a moving visual pattern. Electrodes track the speed at which information moves through your nervous system. - Spinal tap (lumbar puncture)
Your spinal canal is punctured to extract a tiny sample of cerebrospinal fluid for testing. Infections and other illnesses with symptoms similar to multiple sclerosis can be ruled out with the use of a spinal tap.
Treatment
Although multiple sclerosis is incurable, there are many medications available to help you manage the condition. The goal of your therapy plan is to stop the progression of the disease, however, it's important to keep in mind that what is lost in neuronal function cannot be recovered.
Disease-modifying therapies (DMTs):
The medications in this drug class are used for the long-term management of multiple sclerosis. They lessen flare-ups, manage symptoms, and prevent the progression of the illness. Early and aggressive use of these drugs can minimize relapse, limit the growth of new lesions, and perhaps lessen the risk of brain atrophy and disability.
The appropriate medication for you will rely on carefully weighing a variety of criteria, such as the length and severity of your condition, the effectiveness of prior therapies, additional medical conditions, and expenses.
Oral medications
Also called immunomodulators, or sphingosine l-phosphate receptor modulators, are a drug class of medications that work by reducing immune cell activity that might harm nerves.
These medications help prevent neurodegeneration (breakdown of neurons in your brain) or repair damaged nerves and are essential for treating individuals who have multiple sclerosis, particularly those with late-stage progressive multiple sclerosis.
Immunomodulators are also used to control autoimmune damage to your central nervous system (CNS) by minimizing immune cell counts, modifying their activities, or obstructing their exposure to your brain and/or spinal cord. However, these medications do not completely halt disease progression, they only reduce the frequency of relapse symptoms.
- Teriflunomide (brand: Aubagio)
- Fingolimod (Gilenya)
- Dimethyl fumarate (Tecfidera)
- Siponimod (Mayzent)
This once-daily oral medicine has been shown in studies to help slow the course of multiple sclerosis and minimize relapse rates. Additionally, this medication is most commonly used for secondary-progressive. - Dalfampridine (Ampyra)
This medication is a potassium channel blocker that’s used to increase nerve signal conduction to potentially help in improving walking.
Injectable medications
- Glatiramer acetate (Copaxone)
- May help prevent your immune system from attacking your myelin.
- Administered via subcutaneous (SC) injection (underneath your skin) in dosage forms of 20 mg SC or 40 mg SC 3 times per week.
- Interferon betas
- Brands: Avonex (interferon beta-1a) and Betaseron (interferon beta-1b).
- Used by the majority peole with MS.
- May lessen inflammation and promote the development of nerve growth. Can lessen the frequency and severity of relapses. Injected into the muscle (IM- intramuscular) or beneath the skin (SC-subcutaneous).
Infused medications (IV)
- Ocrelizumab (Ocrevus)
- Lowers relapse rates and decreases the progression of the primary- progressive form of multiple sclerosis.
- Alemtuzumab (Lemtrada)
- Lowers yearly recurrence rates and shows MRI benefits.
- 5 days of medication infusions in a row are required, followed by an additional 3 days a year later.
- Natalizumab (Tysabri)
- Lowers relapse rates and lowers the likelihood of impairment, including disability.
- The goal is to prevent potentially harmful immune cells from traveling from your circulation to your brain and spinal cord.
- For some individuals with multiple sclerosis, it could be the first line of treatment, while for others, it might be the second.
For severe attacks, you could consider taking corticosteroids which lessen nerve inflammation. Doctors often administer oral prednisone and intravenous (IV) methylprednisolone.
Common side effects include:
- Insomnia
- Changes in your mood
- High blood pressure
- High blood sugar levels
- Fluid retention
Programs exist to support cognitive and vocational rehabilitation. Physical and occupational therapy programs are available for motor functions, speech, and swallowing.
Although multiple sclerosis is considered an unpredictable disease, the majority of individuals with this condition will continue to lead normal, active lives that are productive because of advancements in therapy. Managing your health and lifestyle can help you get better long-term results.
Related Topics
Generic for Gilenya: Your Key to Affordable Multiple Sclerosis Treatment
Gilenya is a immunomodulator used to control autoimmune damage to your central nervous system (CNS). Gilenya works by minimizing immune cell counts, modifying their activities, or obstructing their exposure to your brain and/or spinal cord. However, Gilenya does not completely halt disease progression, they only reduce the frequency of relapse symptoms.
Read more